PLANTAR FASCIITIS IN RUNNERS: A PAIN IN THE HEEL!
WHAT IS PLANTAR FASCIITIS (FASCIOPATHY)
Plantar fasciitis is an injury around the attachment point of a reinforced fibrous band in the underside of the foot known as the plantar aponeurosis, which is commonly called the plantar fascia.
The symptoms of plantar fasciitis are felt as pain or initially discomfort under the heel, most noticeable on initial weight-bearing in the morning or on standing after prolonged sitting, and immediately after exercise (1). It can be most painful shortly after exercise or on the following morning after running when rising from bed or from sitting. Often activity is initially pain-free or the pain can be ‘run-through’ but as the condition worsens the pain-free time may shorten. The condition is more a degenerative change in soft tissues under the foot rather than inflammatory injury (2).
Unlike most running injuries, this is a problem that isn’t unique to athletic and sports communities and is most common in the age group 40-60 years of age (1). However, it is a common running injury (3,4) reported to account for 7% of running injuries (3) and reported slightly more commonly in women than men (4,5). In runners, it tends to occur at an earlier age but is still unusual before the age of 30. It is associated with increased body weight, the presence of a bony spur (spurs are not the actual cause of the pain), decreased ankle extension range (bending the ankle to move the foot towards the front of the leg, see Fig. 1), decreased big toe joint extension motions upwards, and prolonged periods of occupational standing (1,6). Yet it can also occur without any of these problems. It is not caused by a particular foot type, such as flat feet (pes planus) or high arched feet (pes cavus), turning up in any foot type.
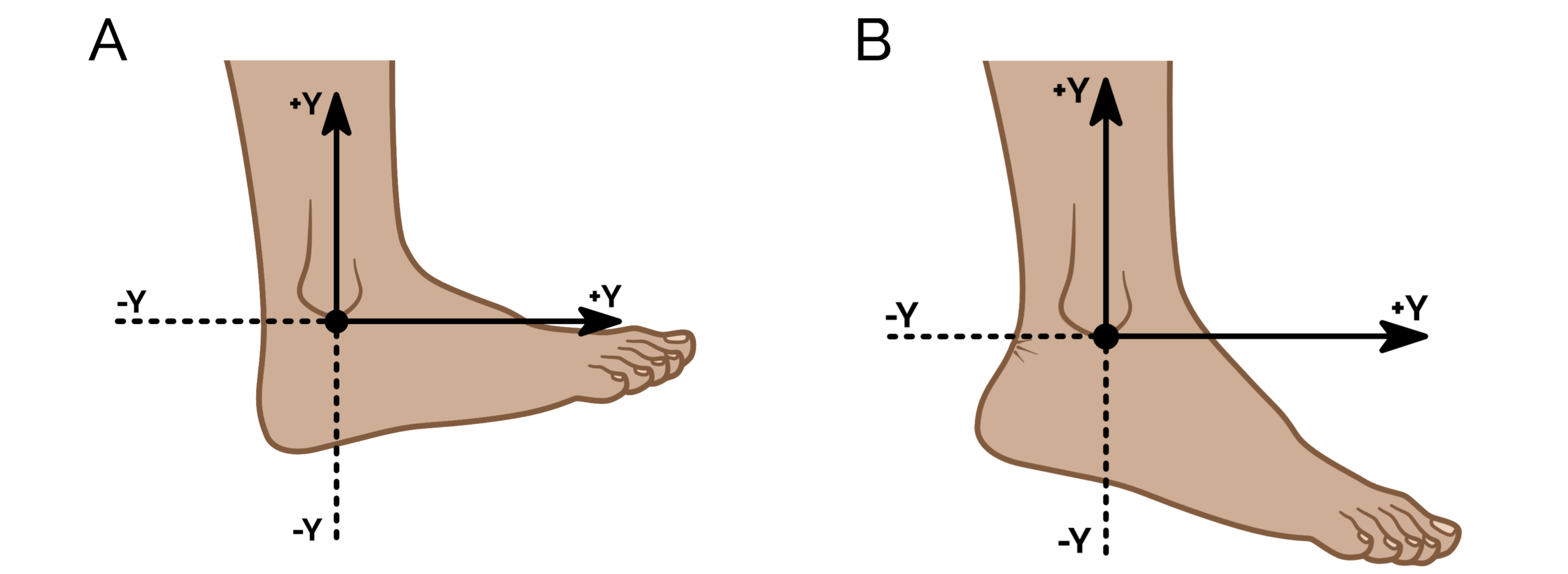 Figure1. Ankle extension (dorsiflexion) is the motion of moving the foot towards the front of the leg (A). It should be freely available. Ankle flexion (plantarflexion) is the movement downward of the foot, which should be a powerful motion (B). Both motions are critically important for normal walking and running and keeping a good range of these motions helps resolve plantar fasciitis and also prevent it.
Figure1. Ankle extension (dorsiflexion) is the motion of moving the foot towards the front of the leg (A). It should be freely available. Ankle flexion (plantarflexion) is the movement downward of the foot, which should be a powerful motion (B). Both motions are critically important for normal walking and running and keeping a good range of these motions helps resolve plantar fasciitis and also prevent it.
WHAT CAUSES PLANTAR FASCIITIS?
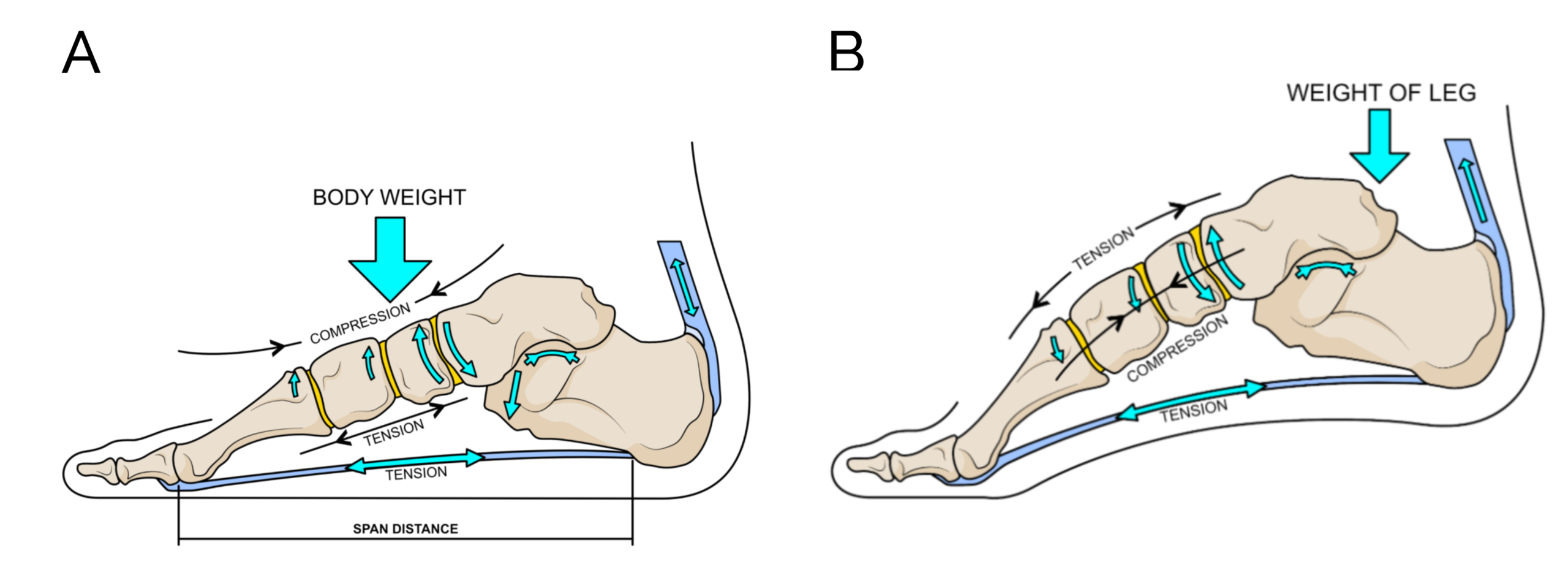
The common explanation is that the causes of plantar fasciitis are multifactorial, which is a nice clinical way of saying there is no one way to develop the condition, but rather there are many ways. The reason for this is the plantar aponeurosis has complex anatomy and function (Fig. 2). 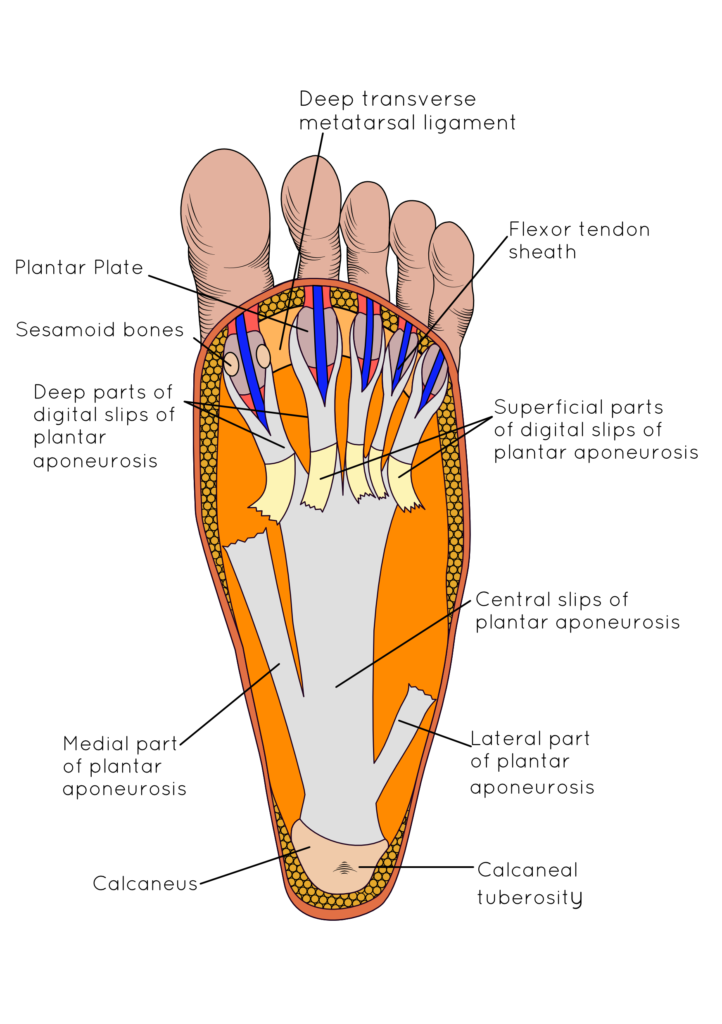 Figure 2. A picture to show the plantar fascia (or aponeurosis) revealing its complex linkages with other important foot anatomy. The muscle of the foot lies under the plantar fascia attached to its deep surface working closely with the plantar fascia to control arch motion.
Figure 2. A picture to show the plantar fascia (or aponeurosis) revealing its complex linkages with other important foot anatomy. The muscle of the foot lies under the plantar fascia attached to its deep surface working closely with the plantar fascia to control arch motion.
It links the heel to the forefoot providing foot ‘arch’ reinforcement and tightens when the toes bend upwards. It also links to the connective tissues that run deep between the muscles under the foot to the ligaments attached to the bones. The plantar fascia is part of a complex link of connective tissues found just under the skin running deep to the bones that allow the foot to change shape on loading and recoil back into shape for the next step. In this role, it assists foot muscles and the changes in foot shape that stiffen the foot for acceleration. With a stiff foot is much easier to drive forward at speed than it would be on a mobile soft foot, just like walking of on hard sand is far easier than soft sand.
Figure 3. By being attached to the heel and the base of the toes, the plantar fascia helps resist lengthening and widening of the foot when the foot is loaded on the ground (A). At heel lift (B) when accelerating off the foot the plantar fascia works with muscle to create a stiff forefoot to provide a stable base for power from the Achilles tendon to push into the ground. The power application is important for walking but occurs under much higher stresses in running. The tightening of the plantar fascia at heel lift that causes the toes to bend upwards is called the windlass effect.
The plantar fascia’s primary job is to help transfer the power from the calf muscles to the forefoot when you lift the heel from the ground and drive forward (Fig.2). To achieve this the plantar aponeurosis uses mechanisms of elastic strength to store energy and stiffen the foot, and then recoil to release energy. It utilises a clever mechanism called the windlass effect that uses the upward bend of the toes occurring as you lift the heel off the ground to help tighten itself and stiffen the foot (7,8) to make it easier to transfer this calf muscle energy to the forefoot. To achieve this the foot also uses muscle power and a curving effect in the front of the foot (9,10). Once stiffened the foot can push hard into the ground using the power from the calf muscles to help your body accelerate with stability to the next step.
This acceleration is obviously faster in running than walking so speed affects the power required from the calf muscles and Achilles. The more power created the more energy that is put into the plantar fascia. The faster we walk or run the more power the plantar aponeurosis has to transfer and the stiffer it has to behave to work properly. The profound complexity of this role is that the process needs the help of muscles in the lower leg and foot, plus ligaments running across the foot to achieve this acceleration job effectively.
Anything that goes wrong in the system can result in the plantar fascia getting increasingly tensioned and stresses. This means that fatigued or weakened calf muscles, foot muscles or damaged ligaments and fascia can all provoke problems in the plantar aponeurosis. The plantar aponeurosis attachment to the heel bone (calcaneus) is most at risk because a join between hard and soft tissues with different mechanical properties represents a weak point. Fascial connective tissue and tendons stretch and recoil elastically, bone is more solid. The heel attachment of the plantar fascia is relatively small in cross-sectional area for a lot of strain to pass through, and thus present a point of force concentration.
WHY HAVE I DEVELOPED PLANTAR FASCIITIS?
A flippant response will be ‘bad luck’! The older you are as a runner the more at risk you become, as you will not be as ‘elastic’ and fatigue resistant as you once were. However, the faster and longer you maintain a run, the greater the risk. This is why older people get plantar fasciitis associated with golf or just daily walking, while in runners it tends to occur at a younger age, often starting after periods of increasing exercise.
If you have weaker muscles or ligaments under the arch of your foot or have injured some of these structures previously you are also more at risk. If you put new demands on the structures on the arch through increased body weight or increasing your running speed or distance you can put more force into your foot arch (remember force = mass x acceleration). Running for a longer time also risks weakening the foot structures through fatigue (11). This is also a risk if you have a job that has you standing for long periods on your feet (1,6).
New running shoes may also be a potential problem if they change the stresses through your foot vault. Lower heels may make it harder to drive power from your calf muscles into the forefoot. Very soft shoes that bend in the middle can change the relationship between the bend in your toes and the power in your calf muscles, while very stiff shoes that won’t bend at the toes can put a lot more stress into your calf muscle to generate power for heel lift. This reflects the principles reported by Takahashi et al (12), where the stiffness of the running shoe is important to acceleration (see Fig. 4), with both too much and too little stiffness being important to running efficiency. Therefore, very soft or very stiff shoes across the forefoot are not good for settling plantar fasciitis but once resolved, using flatter softer more minimalist shoes can help strengthen feet and legs (13).
Figure 4. A stiff shoe is only able to bend at the end of toes, putting more stress on the Achilles tendon and preventing the plantar fascia from working properly which normally through toe bending upwards during acceleration (the windlass effect). This can cause and aggravate plantar fasciitis. Make sure there is some flexibility (but not too much) across the toe joints behind the F indicated in the diagram in your running shoes, as in the picture on the right..
HOW DO I GET RID OF PLANTAR FASCIITIS?
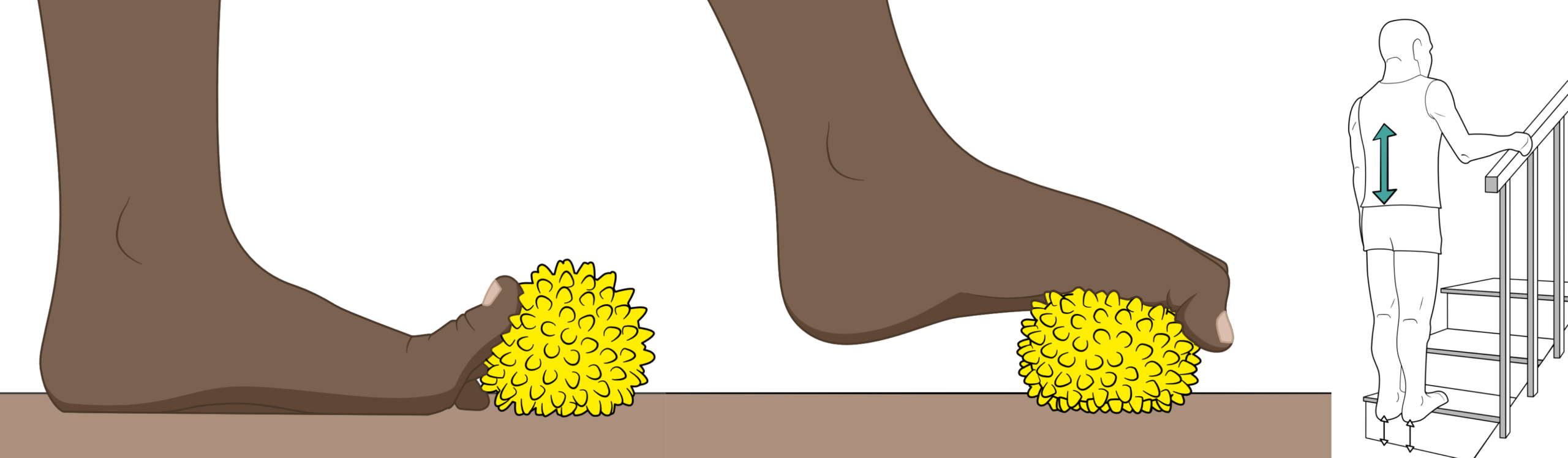
The good news is 90% of runners can resolve this with easy conservative treatments (14) like heel taping, simple plantar fasciitis insoles (no evidence to support expensive custom foot orthoses over more simple pre-made insoles (15) and exercises to strengthen the calf and feet (16,17,18,19). Compression socks also seem to provide relief, particularly for runners.
Figure 5. Using a foot therapy ball can strengthen the muscles under the feet, helping to resolve plantar fasciitis (A & B). Exercises to improve calf strength and flexibility can also aid the recovery of plantar fasciitis (C).
More persistent cases might need extra help from clinical treatments such as mobilisation, manipulation, more specialise exercise/rehabilitation advice, shock wave therapy, steroid or injections, but surgery is truly a last resort.
Beware that other conditions also cause heel pain, including calcaneal stress and heel bone tumours (20), as well as atrophy of the plantar fat pad (21). The symptoms of calcaneal stress fractures are usually significantly more severe, while those of tumours tend to be less consistent than that of plantar fasciitis. The main advice is if your heel pain doesn’t improve after two to three weeks of simple home treatment such as using the HeelFixKit, seek some professional clinical advice. You might need a diagnostic image such as an ultrasound or x-ray if the diagnosis of plantar fasciitis needs to be confirmed from another cause (22).
START TO FIX YOUR PLANTAR FASCIITIS HERE:
https://www.healthystep.co.uk/advice-hub/heel-pain-treatment/
References:
- Irving DB, Cook JL, Menz HB. (2006). Factors associated with chronic plantar heel pain: a systematic review. Journal of Science and Medicine in Sport. 9(1-2): 11-22.
- Petraglia F, Ramazzina I, Costantino C. (2017). Plantar fasciitis in athletes: a diagnostic and treatment strategies. A systematic review. Muscles, Ligaments, Tendons.7(1): 107-118.
- Hill CL, Gill TK, Menz HB, Taylor AW. (2008). Prevalence and correlates of foot pain in a population based study: the North West Adelaide Health Study. Journal of Foot and Ankle Research. 1(1): 2.
- Taunton JE, Ryan MB, Clement DB, McKenzie DC, Lloyd-Smith DR, Zumbo BD. (2002). British Journal of Sports Medicine. 36(2): 95-101.
- Orchard J. (2012). Plantar fasciitis. British Journal of Medicine. 345. E6603.
- Werner RA, Gell N, Hartigan A, Wiggerman N, Keyserling WM. (2010). Risk factors for plantar fasciitis among assembly plant workers. Physical Medicine & Rehabilitation. 2: 110-116.
- Hicks J. (1954). The mechanics of the foot: II. The plantar aponeurosis and the arch. Journal of Anatomy. 88(1): 25-30.
- Caravaggi P, Pataky T, Goulemas JY, et al. (2009). A dynamic model of the windlass mechanism of the foot: evidence for early stance phase preloading of the plantar aponeurosis. The Journal of Experimental Biology. 212(15): 2491-2499.
- Farris DJ, Birch J, Kelly J. (2020). Foot stiffening during the push-off phase of human walking is linked to active muscle contraction, and not the windlass mechanism. Journal of the Royal Society; Interface. 17: 20200208.
- VenkadesanM, Yawar A, Eng CM et al. (2020). Stiffness of the human foot and evolution of the transverse arch. Nature. 579(7797): 97-100. https://doi.org/10.1038/s41586-020-2053-y
- Cowley E, Marsden J. (2013). The effects of prolonged running on the foot posture: a repeated measurement study of half marathon runners using foot posture index and navicular height. Journal of Foor and Ankle Research. 6:20
- Takahasihi KZ, Gross MT, van Werkhoven H, Piazza SJ, Sawicki GS. (2016). Adding stiffness to the foot modulates soleus force-velocity behaviour during human walking. Scientific Reports. 6: 29870.
- Chen TL-W, Sze LK-Y, Davis IS, Cheung RTH. (2016). Effects of training in minimalist shoes on the intrinsic and extrinsic foot muscle volume. Clinical Biomechanics. 36: 8-13.
- Monteagudo M, Maceria E, Garcia-Visto V, Canosa R. (2013). Chronic plantar fasciitis: plantar fasciotomy versus gastrocnemius recession. International orthopaedics. 37(9); 1845-1850.
- Landorf KB, Keenan A-M, Herbert RD. (2006). Effectiveness of foot orthoses to treat plantar fasciitis: A randomized trial. The American Medical Association. 166:1305-1310.
- Hyland MR, Webber-Gaffney A, Cohen L, Lichtman SW. (2006). Randomized controlled trial of calcaneal taping, sham taping, and plantar fascia stretching for short-term management of plantar heel pain. Journal of Orthopaedic and Sports Physical Therapy. 36(6): 364-371.
- van de Water ATM, Speksnijder CM. (2010). Efficacy of taping for the treatment of plantar fasciosis. Journal of the American Journal of Podiatric Medicine Association. 100(1): 41-51.
- Martin RL, Davenport TE, Reischil SF, McPoil TG, Matheson JW, Wukich DK, McDonough CM. (2014). Heel pain-plantarfasciitis: Revision 2014. Journal of Orthopaedic and Sports Physical Therapy. 44(11): A1-A23.
- Huffer D, Hing W, Newton R, Clair M. (2017). Strength training for plantar fasciitis and the intrinsic foot musculature: A systematic review. Physical Therapy in Sport. 44-52
- Monteagudo M, de Alboronz PM, Gutierrez B, Tabuenca J, Alvarez I. (2018). Plantar fasciopathy ; a current concepts review. EFORT Open Reviews. 3(8): 485-493.
- Yi TI, Lee GE, Seo IS, Huh WS, Yoon TH, Kim BR. (2011). Clinical characteristics of the causes of plantar heel pain. Annuals of Rehabilitation Medicine. 34(4): 507-513.
Hormozi J, Lee S, Hing DK. (2011). Minimal invasive percutaneous bipolar radiofrequency for plantar fasciopathy: a retrospective study. The Journal of Foot and Ankle Surgery. 50(3): 283-286.