When Stubborn Heel Pain Isn’t Plantar Fasciitis
Playing O’s and X’s with your plantar heel, can help start the process of forming a diagnosis. Let us explain.
 Heel pain is a common symptom. Heel Pain has been reported to constitute 25% of all MSK foot symptoms , most of which are plantar heel pain. It is proposed that changes in people’s lifestyle and activities, particularly as they get older are influencing the development of heel symptoms. It has been estimated that 10% of the population will experience an episode of heel pain during their lifetime (Van der Water & Speksnijder, 2010), but has been reported in up to 25% in more athletic populations (Ribeiro et al, 2011) and has been noted as common among workers who stand for long periods (Werner et al, 2010).
Heel pain is a common symptom. Heel Pain has been reported to constitute 25% of all MSK foot symptoms , most of which are plantar heel pain. It is proposed that changes in people’s lifestyle and activities, particularly as they get older are influencing the development of heel symptoms. It has been estimated that 10% of the population will experience an episode of heel pain during their lifetime (Van der Water & Speksnijder, 2010), but has been reported in up to 25% in more athletic populations (Ribeiro et al, 2011) and has been noted as common among workers who stand for long periods (Werner et al, 2010).
People like to try to self diagnose their heel pain (usually via google) or you may only have seen a general practitioner regards their symptoms, both of which usually results in a diagnosis of plantar fasciitis. Problems in attempting to treat’ heel pain begin with the popularity of the term plantar fasciitis as a universal diagnosis for plantar heel pain. I have always preferred the ‘..say what you see’ approach, which Stephen Mulhern (or Roy Walker as I remember it!) uses to help the contestants on Catchphrase, and plantar heel pain does describe the symptom nicely. However, there is more than one potential diagnosis for this symptom.
Symptoms – location, type of pain
Symptoms of plantar heel pain can vary according to the cause, and certain signs are expected in ‘plantar fasciitis”. These are:
- First step(s) pain – rising from bed in the morning or from a period of sitting.
- Improves with walking, unless activity sustained for longer periods.
- Pain can be described as aching, throbbing and occasionally lancinating (occasionally stabbing).
- Pain can be diffuse and migratory but is generally localised to an area 1-2 cm around the medial process of the plantar calcaneal tubercle.
- Insidious onset.
- Often worse in flat shoes or barefoot.
- Pain most around heel lift.
Symptoms that indicate fat pad atrophy – location, type of pain
Plantar fat pad atrophy is a quite common condition, more common with age, vascular disease and diabetes. It results in changes in both the fat cells that enclose the fatty tissue. Primary symptoms are:
- Deep generalised ache or bruised feeling on weightbearing.
- Worse walking on hard ground, barefoot or thin-soled shoes.
- Pain central but diffuse in the heel.
These symptoms are not unique to heel fat pad atrophy and are very similar to those initiated by a locked or arthritic subtalar joint, but they are distinct to plantar fasciitis symptoms. This should be a clue to consider other diagnoses than plantar fasciitis.
 This article is for people that staunchly believe they have PF or have been advised or receiving treatment for PF with unresolved symptoms, yet do not demonstrate the classical symptoms.
This article is for people that staunchly believe they have PF or have been advised or receiving treatment for PF with unresolved symptoms, yet do not demonstrate the classical symptoms.
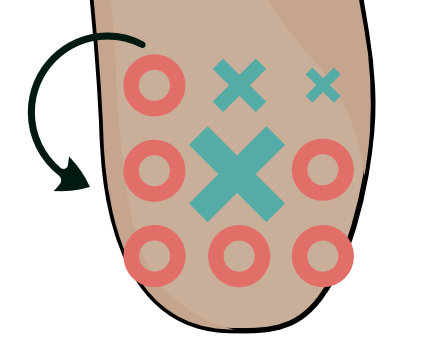
When examining the heel, consider your heel as an O’s and X’s board and work your way around pressing firmly around the fat pad.
While you examine the heel note the quality of the fat pad. If the fat pad feels particularly compliant (soft, malleable, watery), migrates sideways easily on pressing, or you can feel the bony surface of the heel bone, then perhaps the heel fat pad is incapable of dealing with impact on heel contact. If so the bone can become bruised, filling with extra fluid (oedema).
Pain right in the centre of the heel doesn’t usually indicate PF, as this is not the primary location for the condition.
Symptoms associated with fat pad atrophy tend to be central, but also more diffuse than plantar fascial symptoms. Usually, you’ll be able to feel the calcaneal plantar tubercle in the centre of the heel, which can feel bruised.
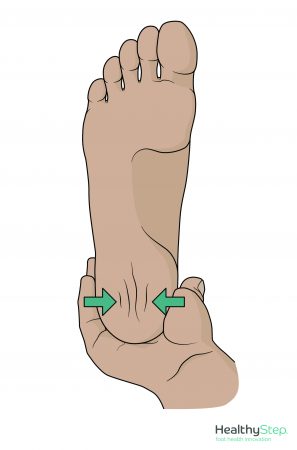 If squeezing the sides of the heel/calcaneus produces pain, the diagnosis is likely to be linked to calcaneal oedema. This can occur in a number of conditions, such as calcaneal stress fractures, locked or degenerate subtalar joints, or in children Sever’s. If plantar fat pad atrophy has been an issue for a sustained period over 6 months, then oedema can also develop, but it is a very rare finding associated with plantar fasciitis
If squeezing the sides of the heel/calcaneus produces pain, the diagnosis is likely to be linked to calcaneal oedema. This can occur in a number of conditions, such as calcaneal stress fractures, locked or degenerate subtalar joints, or in children Sever’s. If plantar fat pad atrophy has been an issue for a sustained period over 6 months, then oedema can also develop, but it is a very rare finding associated with plantar fasciitis
After locating the heel pain on direct plantar pressure, try squeezing the plantar fat pad together. If the pain disappears, maintain the position of the fat by keeping the squeeze going then press back into the fat pad. Still no pain? Release the fat pad and press again. If the pain has returned you can be pretty sure you are dealing with fat pad dysfunction.
Should we expect treatment programmes designed for plantar fasciitis work for conditions such as fat pad atrophy? Probably not.
Will these symptoms respond to a steroid injection?
If fat pad atrophy is diagnosed, steroid is contraindicated. Calf stretches are not going to help. And rigid shell foot orthoses will irritate.
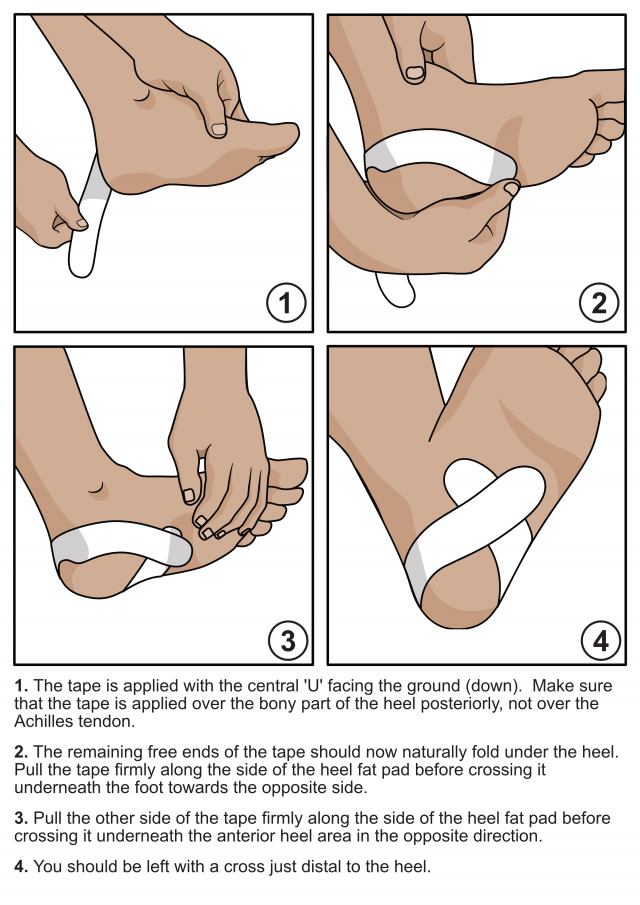
However, heel taping can help tether the soft tissues in place under the heel, and restrict fat pad spread on loading the foot. This can help provide some short term reestablishment of normal heel pad viscoelastic properties while the tape is in place. The HeelFixKit tape is an excellent option here because it is simple and easy to apply.
Fat pad atrophy will also benefit from:
- Soft cushioning under the calcaneus, for heel strike and for long periods of standing – Pressure perfect insole and gel cushions are very helpful (not the teardrop-shaped blue spots though).
- Protection at all times, avoid barefoot, especially on hard surfaces – wear soft cushioned footwear inside the house.
- Compression of the heel pad area with good hosiery such as our Foot Pump Sock range.
- Cushioned trainers with torsion stability and a firm heel counter (applying sideways heel pressure) with internal cushioning orthosis (not memory foam).
- Longer-term use of supportive, yet cushioned orthoses such as the Pressure Perfect because the heel cup and the midfoot saddle apply fat pad stabilisation constrain the fat pad spread as well as offering plantar cushioning.
- Cushioned rubber-type clogs with an inbuilt heel cup (think like alligator…you know the ones) in the house, the best ones have a degree of heel lift . Make sure they aren’t too old.
A dedicated regime of taping and cushioning for a few weeks should settle symptoms, but the patient will need long term protection.
The reason is an atrophic heel fat pad that has lost its normal viscoelastic properties. An atrophic heel pad is too compliant on impacting the ground having too much ability for the fat to flow away from the load (too much viscosity). The atrophic heel fat pad is also unable to recoil back into shape normally after loading (lacks elasticity). The result is an atrophic heel fat pad that cannot dissipate impact energy and instead allows that energy to be transferred into the deeper structures where is causes pathology.