Achilles Tendinitis/Tendinopathy: The pain behind the ankle/heel!
Introduction
Achilles tendinitis is one of the most common problems in the leg. Approximately 6% of people report Achilles tendon pain during their lifetime, but among recreational runners, it is as high as 56%. It is most commonly found in people between the ages of 30 and 55. This is when tissues are starting to become ‘aged’ and yet people are usually still very active.
It results from a combination of degenerative changes and inflammatory responses that can occur across the length of the tendon. Achilles tendinitis has several different causes. In clinical circles, Achilles pathologies tend to be referred to as Achilles tendinopathy to indicate it is more than just Achilles inflammation, something its common name suggests.
Achilles pains tend to be first noticed after longer periods of exercise below the calf and behind the ankle and heel. The Achilles area can also feel stiff and/or slightly tender when first moving after rest, particularly on a day after higher levels of exercise. Over time, symptoms become associated with all weight-bearing exercises, such as during periods of longer walking or running. If untreated, the affected limb’s ankle power can gradually weaken, making higher-speed gait activities harder to perform.
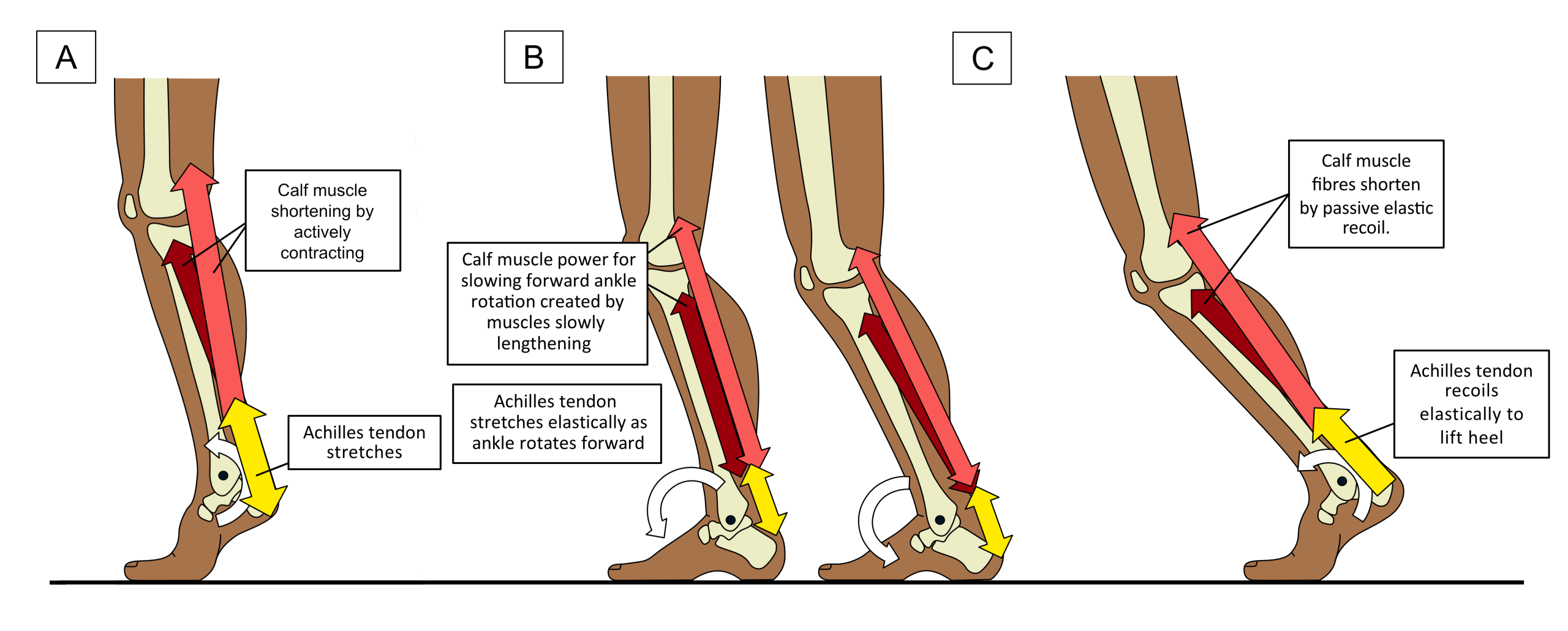
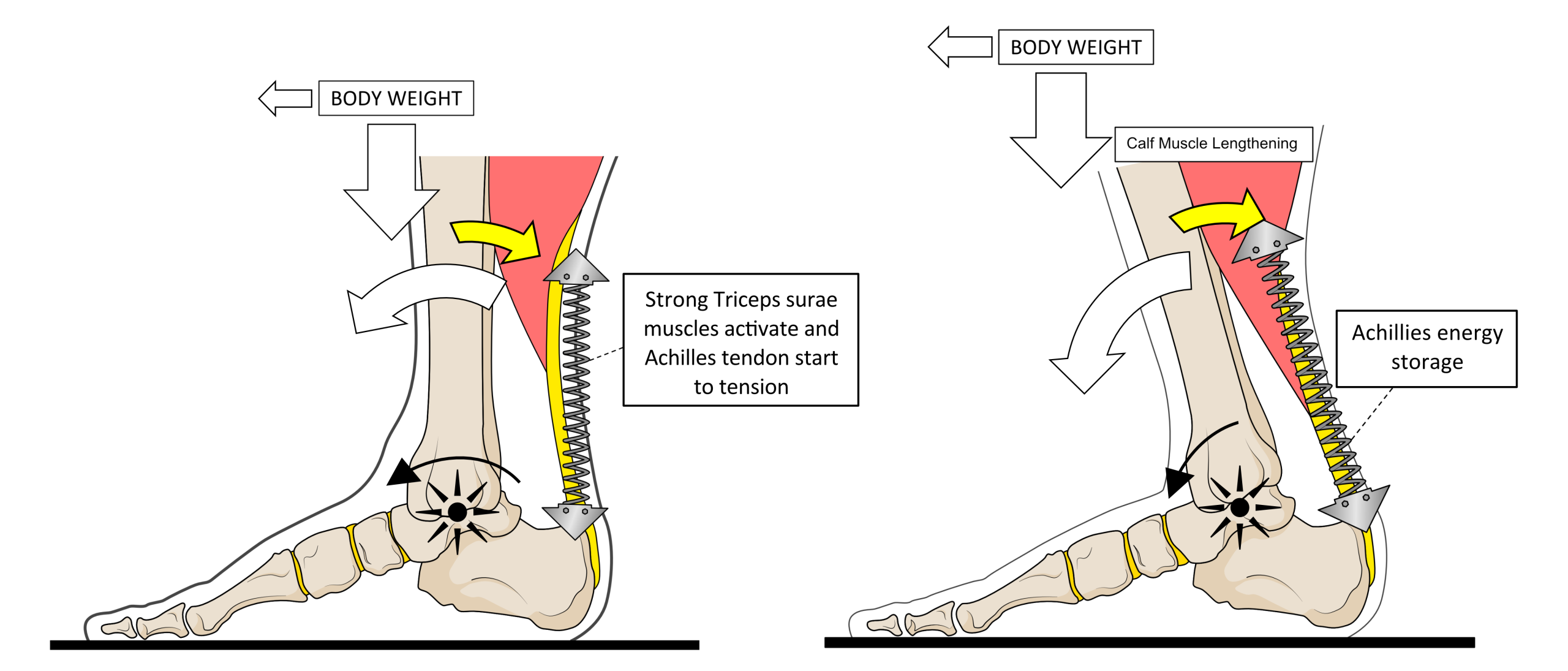
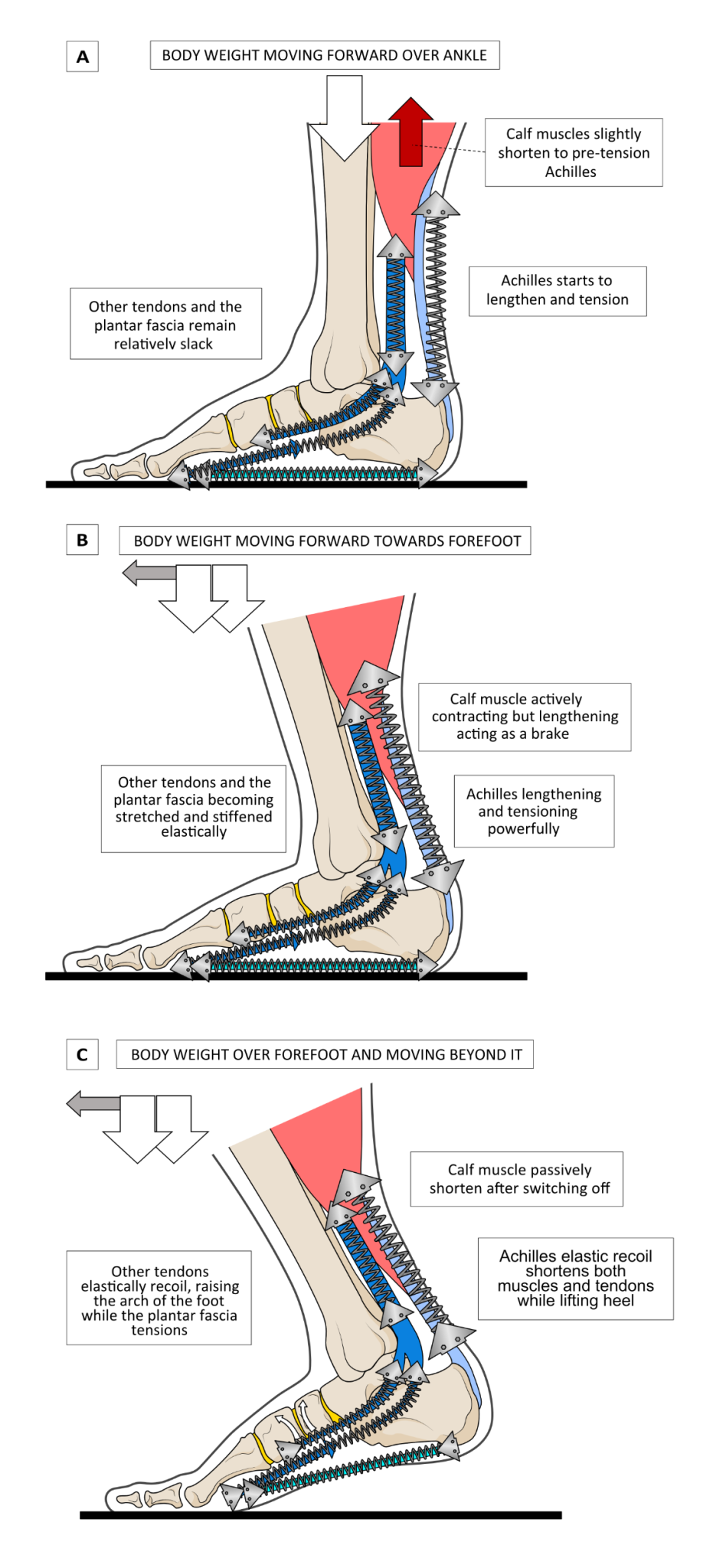
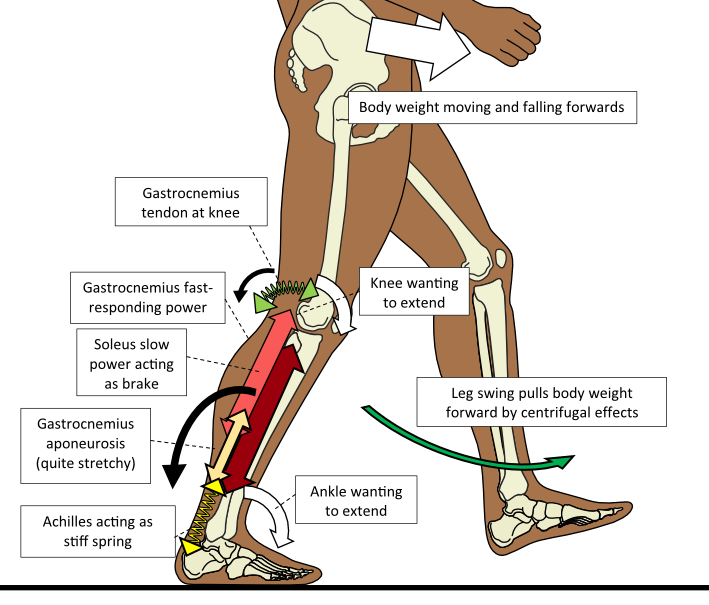
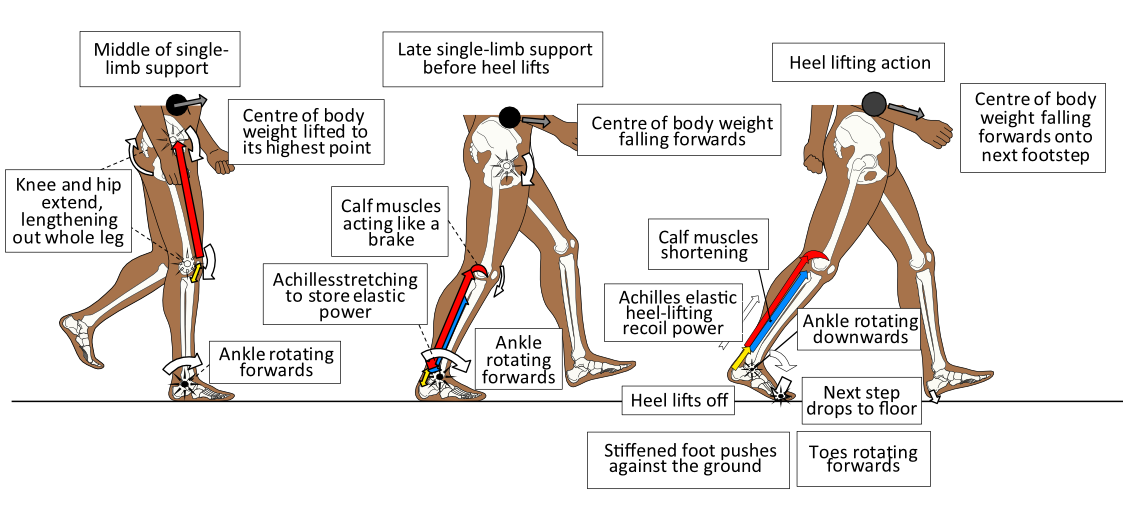
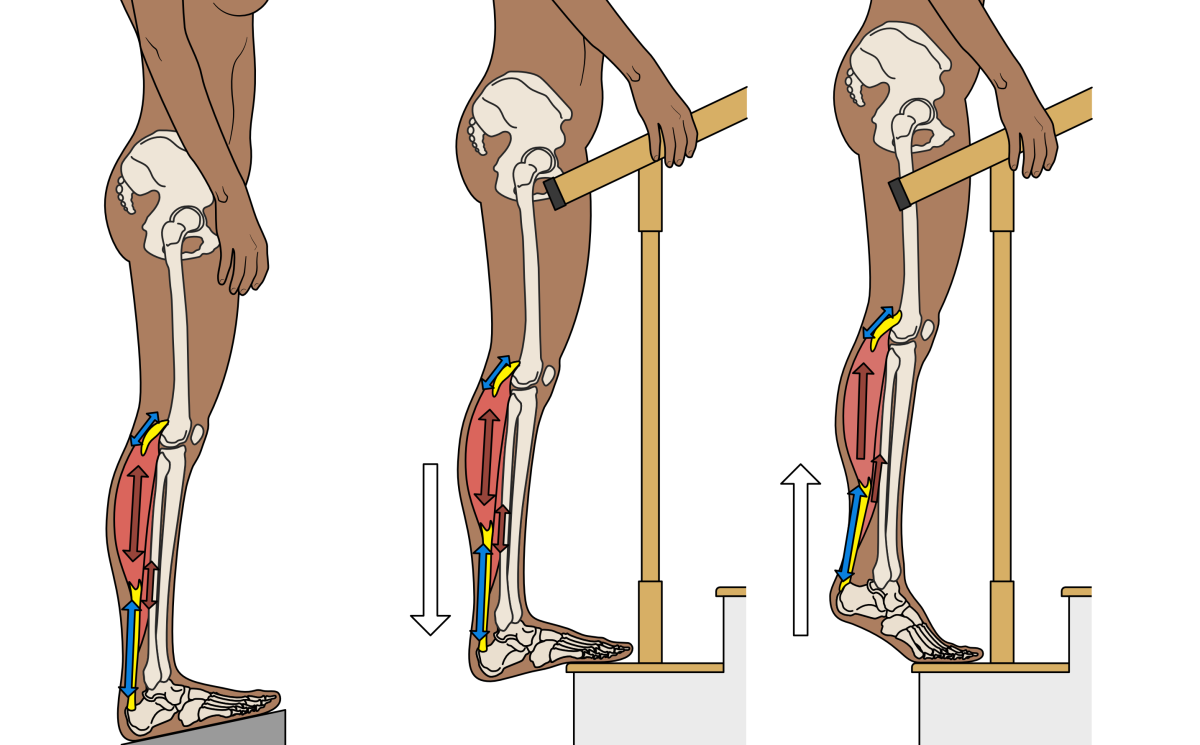
The Achilles is a very strong tendon. It allows powerful calf muscles to control motion around the ankle, behaving like a stiff spring. When the ankle rotates forward (effectively moving the foot nearer to the front of the shin) both the calf muscles and Achilles lengthen and tension. When calf muscles contract and shorten, they pull the foot downwards at the ankle. If calf muscle power is sufficient, the heel will lift off the ground. This tiptoe heel-raising action causes the spring-like Achilles to lengthen and stretch under tension as the muscles contract and shorten. However, during gait the action of lifting the heel does not occur by active muscle contraction, but from the elastic recoil of the Achilles being stretched prior to the moment the heel lifts. The Achilles shortens under the power of elastic recoil, lifting the heel and passively shortening the muscles as it does so. This difference is demonstrated in Fig. 1.
Figure 1. Rising up on tiptoe (A) uses the Achilles quite differently than during human locomotion. When walking, the ankle rotates forward to move body weight over the foot (B). This action stretches the Achilles loading it will elastic-recoil power. This is then released as the heel lifts (C) which removes the requirement for heel-lifting muscle power.
During walking and running, the body weight passes over the weight-bearing foot as we move from step to step. As the ankle rotates forward (an extension motion, called dorsiflexion), the Achilles becomes increasingly stretched. Once body weight has moved away from the heel and over the forefoot, the stretched Achilles starts to elastically recoil to lift the heel off the ground. This elastic recoil causes both the Achilles tendon and the calf muscles to passively shorten. This is why the normal action of heel lift does not require muscle activity. The Achilles ‘springs’ us towards the next step. This is very mechanically efficient and makes running and walking much easier. This efficient spring-loaded action gives an indication as to why having problems with the Achilles is a big issue.
Types of Achilles Tendinitis
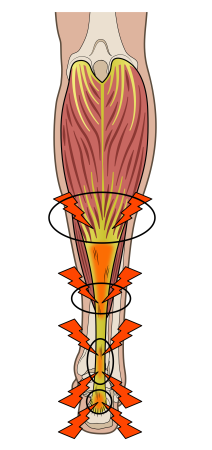
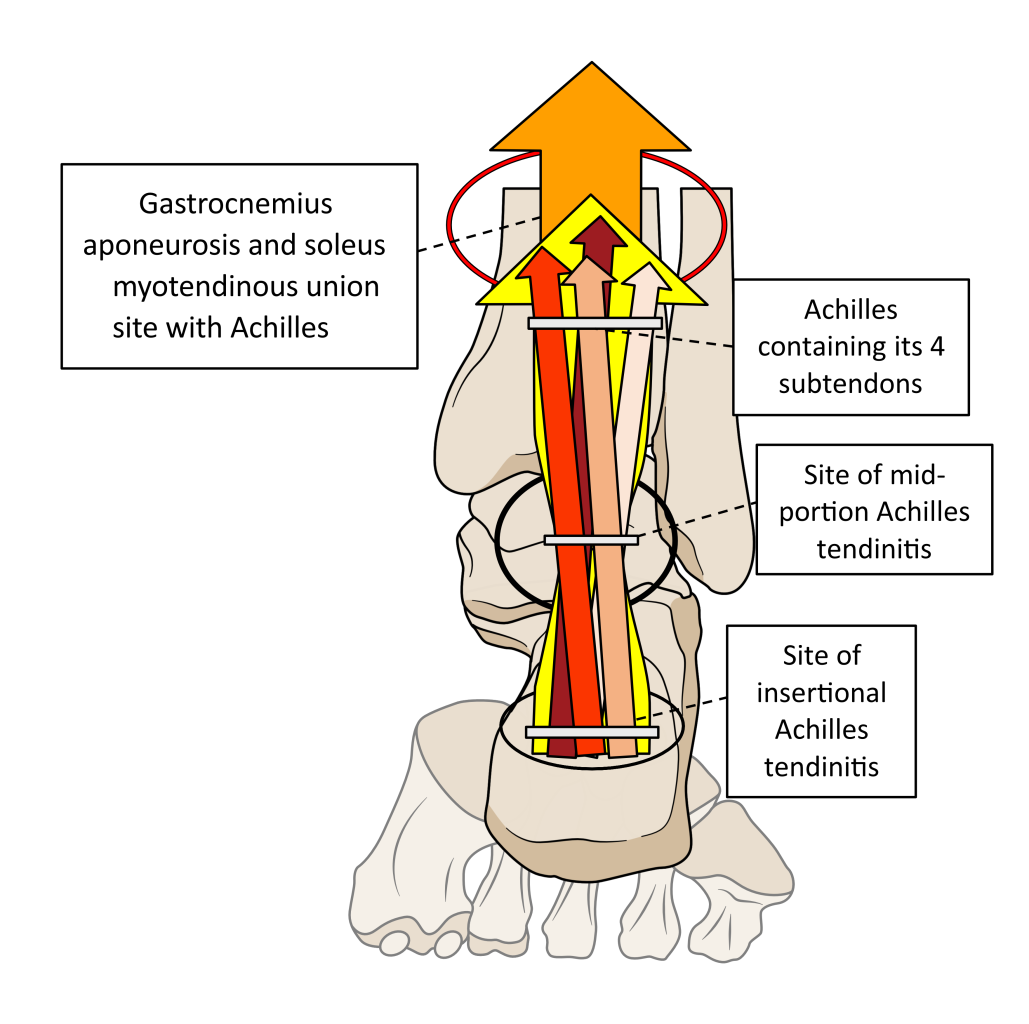
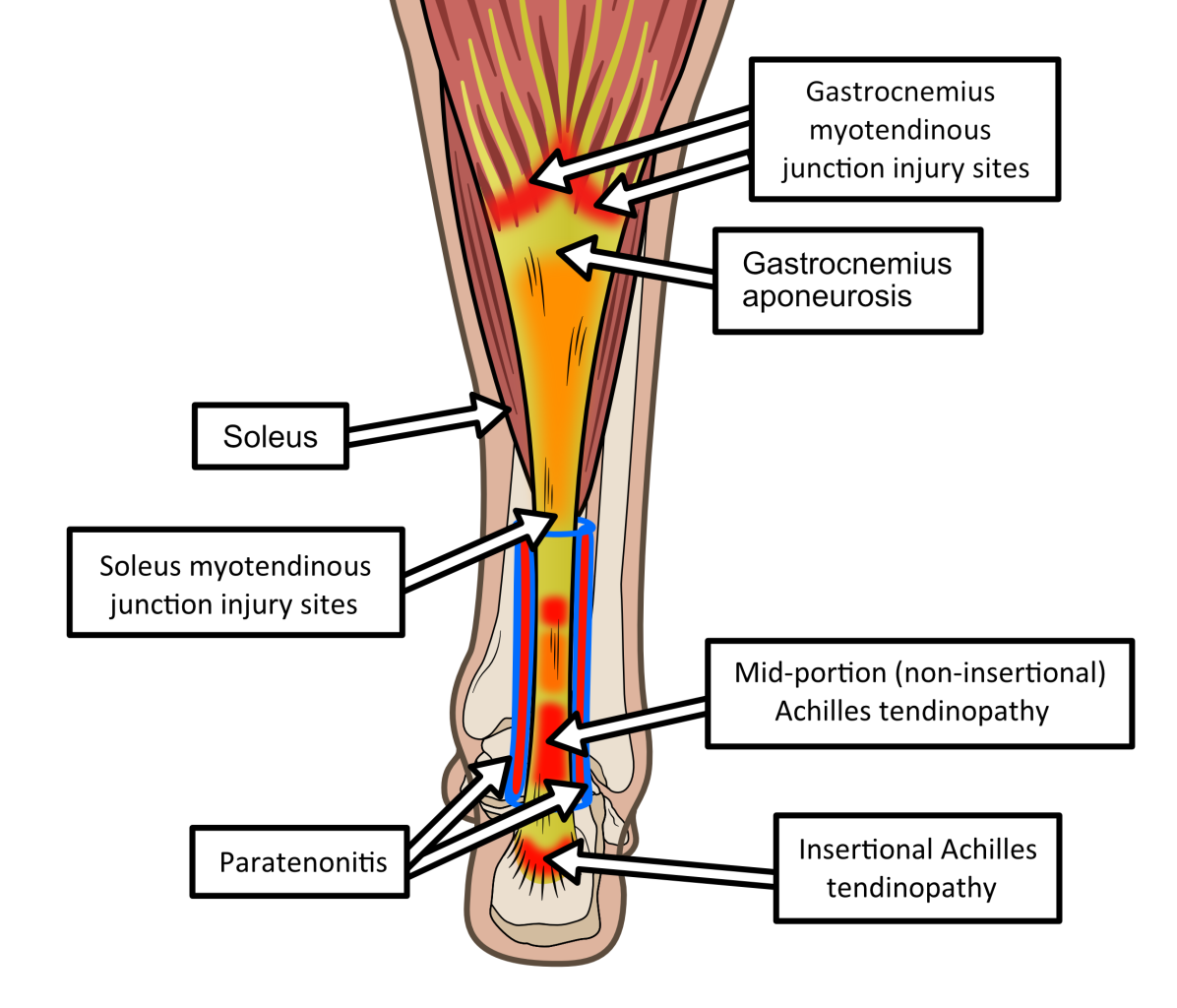
To understand any particular tendonitis, it is important to know what part of the Achilles is failing. Achilles tendinitis is subdivided into different types. Sometimes it is caused by the fluid-filled fibrous covering of the tendon becoming inflamed. This is known as Achilles paratenonitis. Sometimes injury focuses to the join between muscle and tendon fibres known as the myotendinous or musculotendinous junction. However, the most important division of Achilles tendon problems is into those affecting the main body of the tendon, known as mid-portion or non-insertional tendinitis, and those affecting the bone attachment area, known as insertional tendinitis. See Fig. 2 for the locations of these issues.
Figure 2. The locations of common Achilles tendon problems.
Occasionally, insertional Achilles problems arise from autoimmune inflammatory diseases rather than mechanical overloading. Examples include Reiter’s or psoriatic arthritis. Such conditions are best managed by a rheumatologist, although symptoms can be improved by heel-lifting insoles to some extent. These conditions should be easily identified as the cause of the problem by a clinician/therapist through careful history taking.
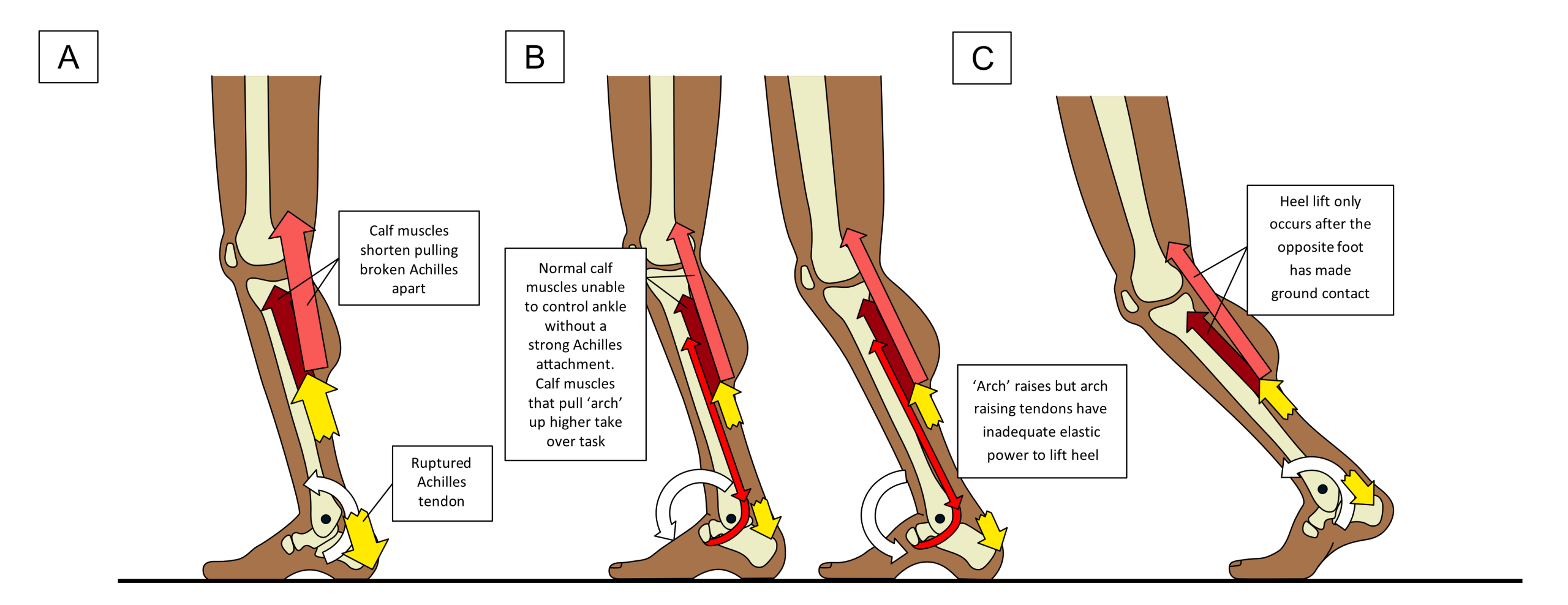
Sometimes the Achilles tendon can rapidly tear. Achilles tendon rupture or partial rupture are associated with sudden loss in ankle power after a single moment of sharp pain. This is often accompanied with a sensation of something hitting the back of the ankle. Explosive power activities with rapid changes of direction such as tennis and squash, are commonly associated with ruptures. Traumatic events such as falling backwards down a step with the foot in a very extended/dorsiflexed (upwards) position can also cause ruptures. Achilles ruptures causes an inability to create any controlling power around ankle motion as indicated in Fig. 3.
Figure 3. When the Achilles is ruptured, the calf muscles are unable to lift the heel off the ground. Standing on the affected leg and attempting to go on tiptoe reveals the problem (A). In gait, the slowing of ankle rotation by the usual calf muscles cannot be achieved, so other calf muscles take on the role. These muscles primarily lift the ‘arch’ so instead of the foot flattening before heel lift, the arch profile rises up (B). This slows ankle rotation but makes it harder to lift the heel. As a result of this and the loss of the Achilles elastic recoil power, heel lift is delayed until the other foot is fully on the ground (C). Raising the heel is then produced by hip muscle power.
If you cannot rise up on tiptoe after a sudden pain or an impact-like sensation at the back of your heel, please see a clinician/therapist urgently for assessment. The assessment is easily performed by an experienced clinician by simply squeezing the calf muscle and watching ankle motion, by using a soft ultrasound scan or ideally, through both tests.
Ruptures are uncommon in people with histories of Achilles pains. Instead, ruptures tend to happen to people without warning during activities involving high calf muscle power or large ankle upward motion. Once pain starts in the Achilles, the body reacts to protect it, reducing stresses upon it. This prevents stresses from reaching a level that could rupture it. Without pain, the body can be unaware that high forces are being loaded into a degenerate tendon, which can then result in it suddenly breaking because the body hasn’t taken action to protect it. The Achilles has few pain fibres, so it relies on surrounding tissues to alert us to Achilles injuries.
Children with Achilles-like pains
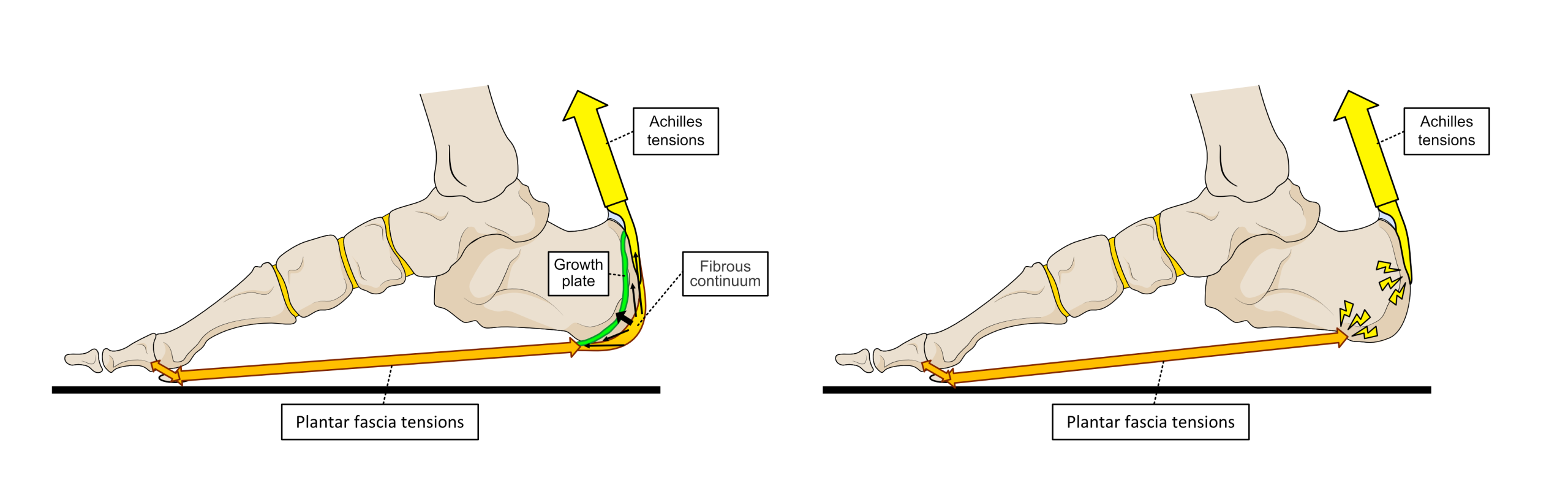
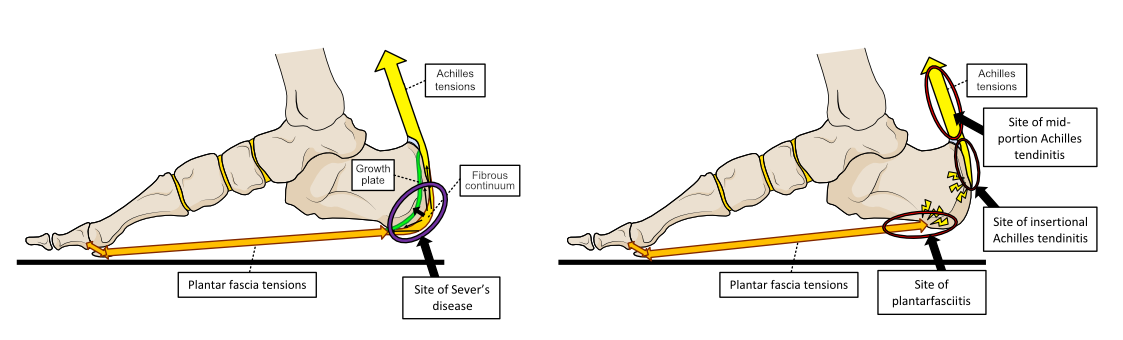
Children with posterior heel pain associated with exercise, should not have Achilles tendinitis. Instead, they have a condition known as Sever’s. This is triggered by excessive stresses within the area between the Achilles and a strong fibrous band under the foot, called the plantar fascia. In children, the fibres from these two structures link together around and under the heel bone (calcaneus). Children also have an area of immature growing bone within the heel which can lead to stresses irritating around it. The fibre continuation is lost between the ages of 20 and 30. In mature adults, all forces focus on the attachments of the Achilles and plantar fascia to the bone. Both of these areas are associated with injury and degeneration, called Achilles tendinitis and plantar fasciitis. These conditions do not normally affect children. Fig. 4 indicates the difference between immature and mature Achilles and heel bone anatomy.
Figure 4. In children (left image) the heel anatomy is quite different to mature adults (right image).
Why is the Achilles tendon so important?
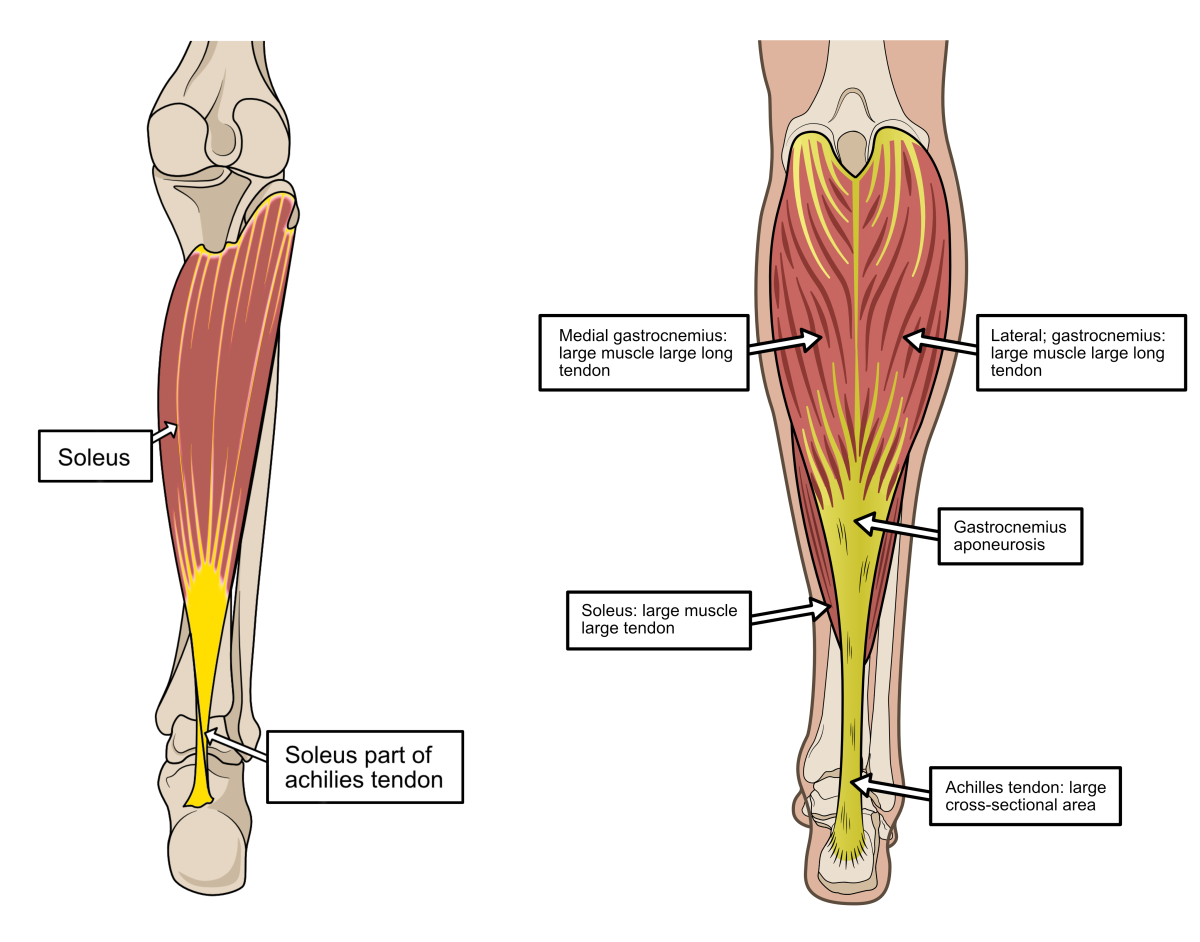
The Achilles is the largest tendon by cross-sectional area (thickness) in the human body, making it easy to feel at the back of the ankle. Its size is very important and indicates its strength and the amount of force it is required to handle. The Achilles tendon is unusual because it operates under stresses close to its material strength. Stresses can be as high as eight times body weight. However, it uses a number as special constructional tricks to prevent its failure.
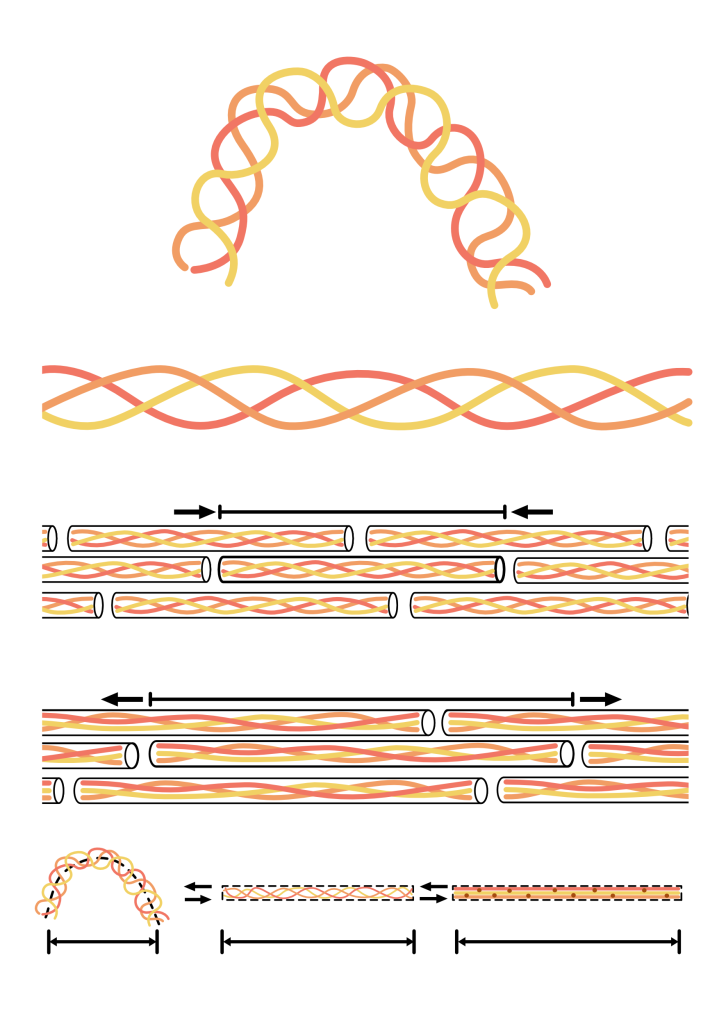
The Achilles is a special type of tendon, known as an energy-storage tendon. These tendons rely on the fibrous bundles within them being able to slide freely past each other, with the biological glue between the fibres being springier than that found in most tendons. Thus, energy storage tendons are more stretchable, elastic, and fatigue-resistant as a result.
The Achilles is therefore incredibly thick and elastic in comparison to other tendons. Most tendons can strain (lengthen) by between 15-22% before they fracture. However, the Achilles can achieve strains up to 18-28% before failure, and then return far more of its stretch energy back as elastic recoil. This is very much like a mechanical spring as demonstrated in Figs. 5 and 6.
Figure 5. When standing, body weight lies just in front of the ankle and wants to fall forward (left image-white arrow). Acting like a spring, the Achilles tensions and resists the body weight’s fall, pulling it slightly backwards (yellow arrow). This spring-like tension helps keep an erect body posture without requiring muscle activity. When the ankle bends forward during walking (right image), the Achilles is stretched elastically loading it with recoil energy. Under calf muscle activity, this elastic recoil power acts like a brake (yellow arrow) on forward motion of the ankle (white arrow).
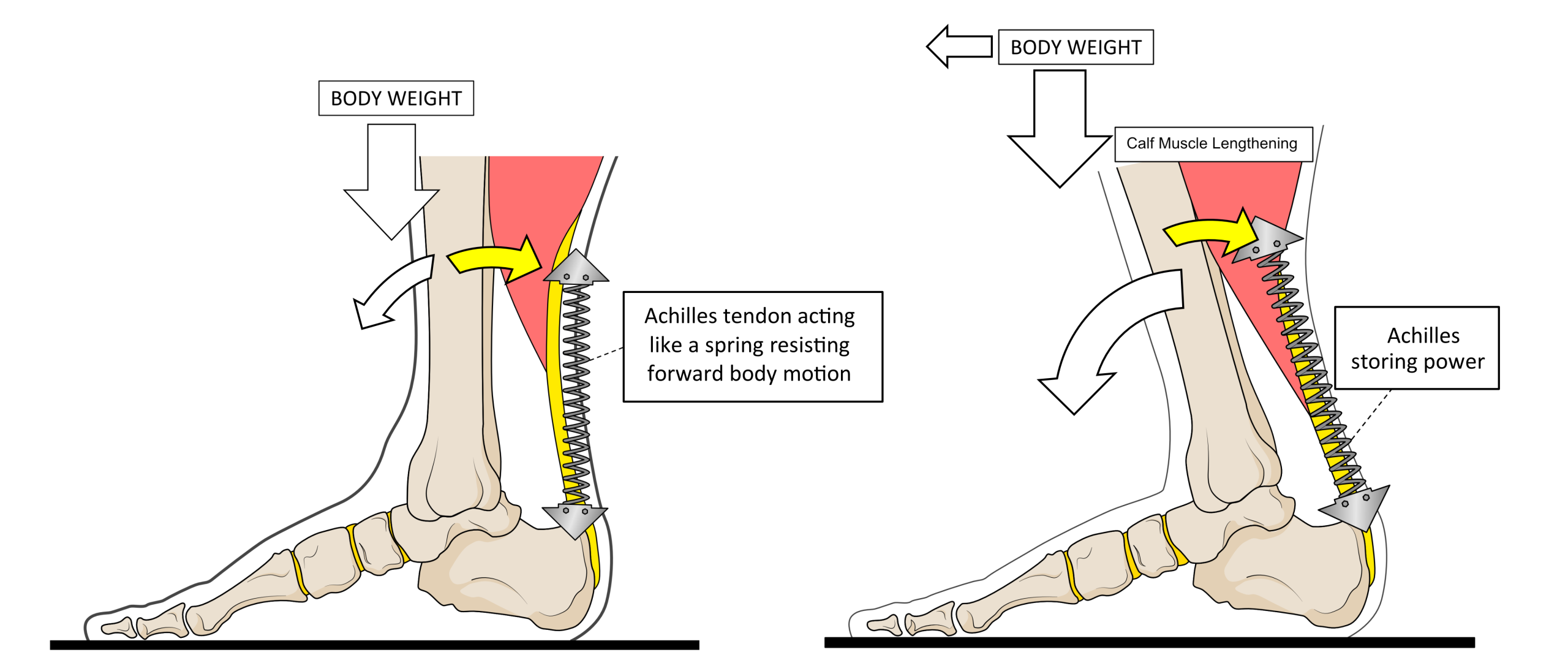
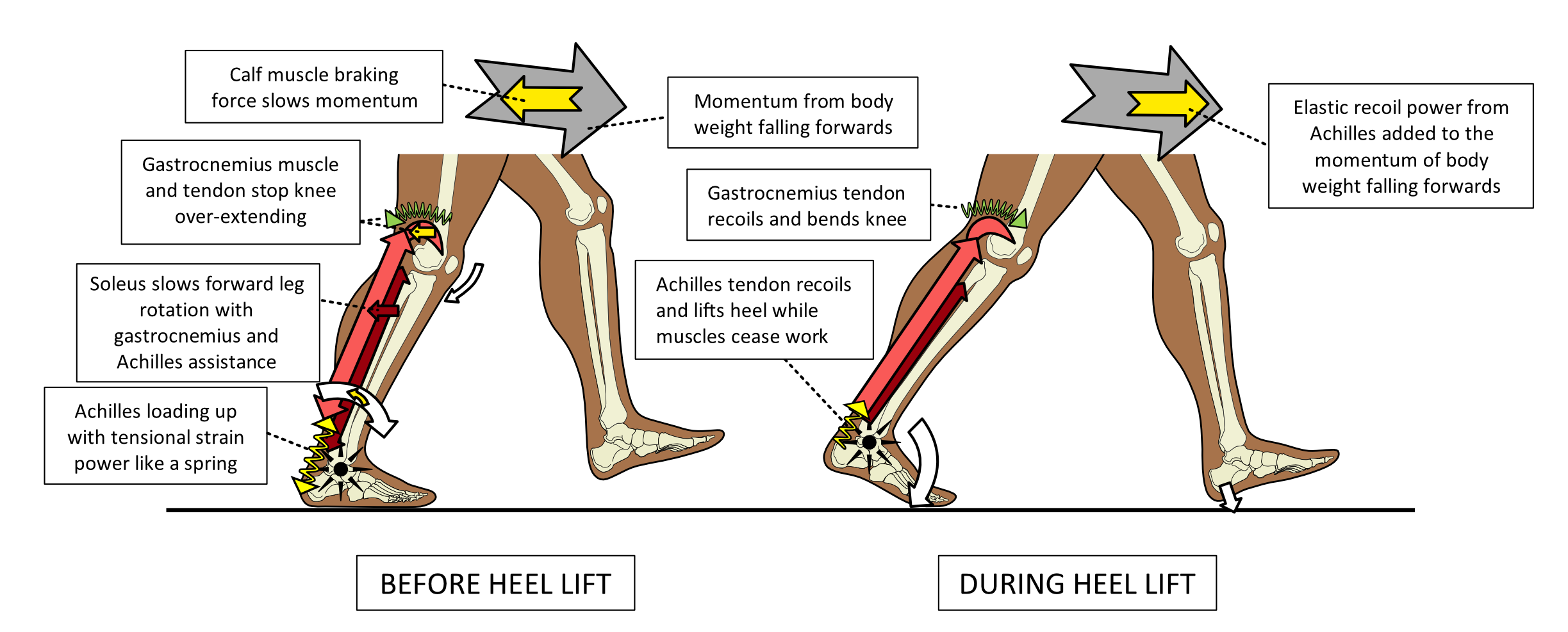
During walking and running, the Achilles tendon is loaded with very high forces as a result of our unique form of gait. Our body weight passes over one ankle on a single long weight-bearing limb, one at a time. Stresses are particularly high during the second half of the foot weight-bearing period when bodyweight moves in front of the ankle. It is during this later period of walking that the Achilles tendon is loaded with lots of force that powerfully stretches it. This is because the Achilles and calf muscles are used to control body weight rotating forward over the foot, acting like a brake to slow forward momentum. The strong braking action on the body weight loads the spring-like Achilles with lots of potential elastic-recoil power, as shown in Fig. 6.
Figure 6. As body weight moves in front of the ankle in walking, the calf muscle starts to become highly active (left image). This starts a tensioning process on the Achilles which increases as the calf muscles’ power acts as a brake, (yellow arrows). Both the calf muscles and the Achilles lengthen before heel lift to control motion (right image).
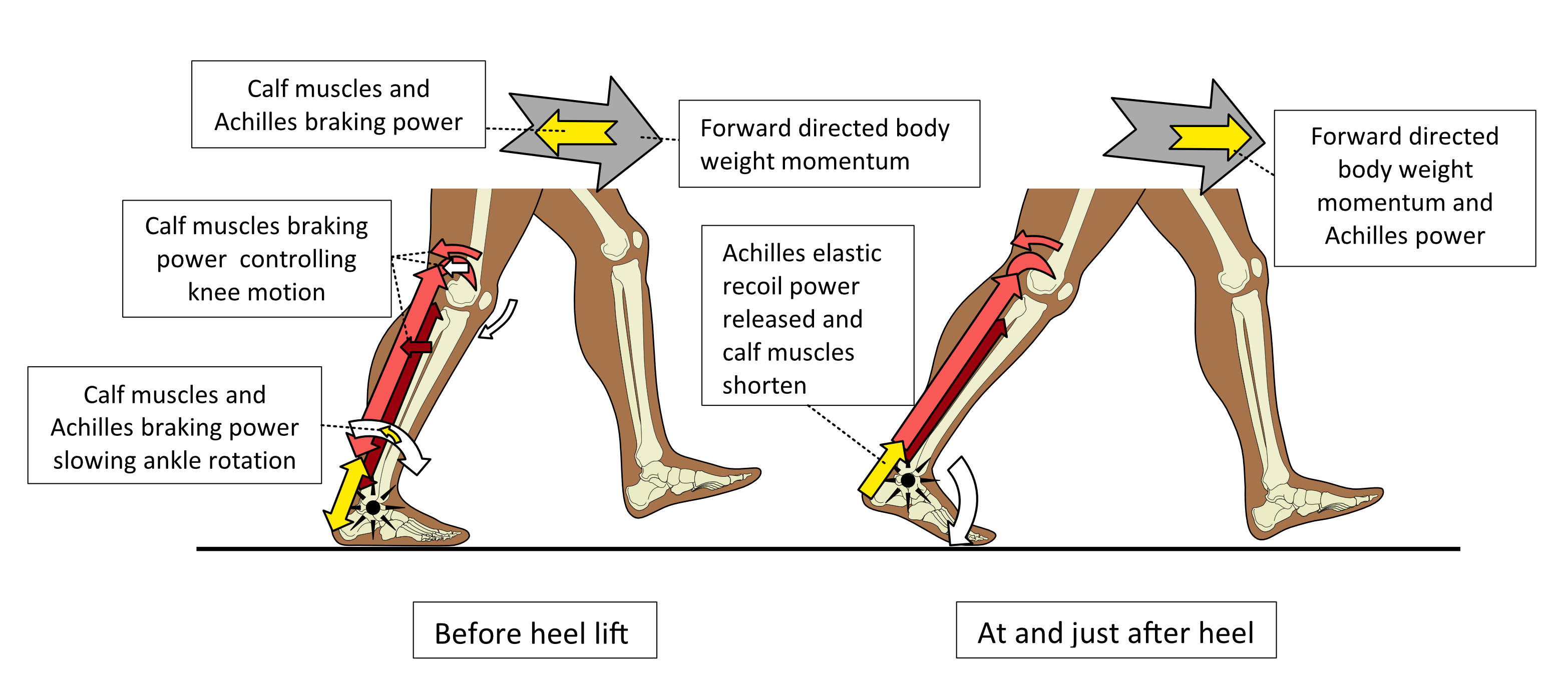
The elastic stretch on the Achilles is released as recoil heel-lifting power once body weight has moved over the forefoot. This power provides acceleration to help drive our body weight forward towards the next step. Thus, momentum is maintained while moving onto the next foot from the recoil power from the Achilles. The braking action before heel lift and the act of heel lifting to spring forward, explains why the Achilles is so important. Figure 7 shows this relationship.
Figure 7. The period where the body weight is in front of the ankle before heel lift, permits body weight to fall forwards and slightly downwards (grey arrow). This requires the calf muscle to create braking forces (yellow arrows) by gradual lengthening under Achilles tension. This prevents the body from rotating forward too quickly and elastically stretches the Achilles. Once the body weight has moved over the forefoot, the Achilles elastic recoil power is released, causing the heel to spring up to create heel lift. The leg swinging forward rapidly drops onto the ground as a result of the heel lift.
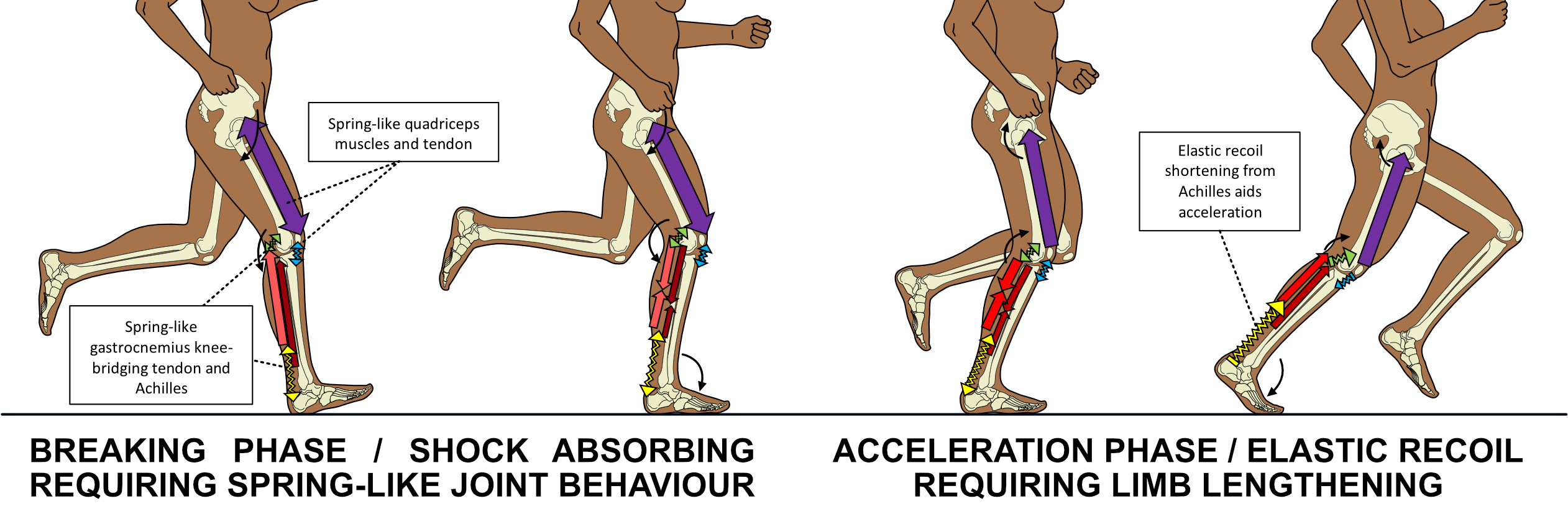
In running, elastic-recoil power storage in the Achilles becomes even more important to maintain momentum and speed. The Achilles makes far more length changes than do the muscles during running compared to walking. As a result, the Achilles has to behave more elastically, requiring it to operate under greater tensional strains from the moment the foot first touches the ground. This increases the stresses within the Achilles compared to walking, with the amount of stress related to the running speed. Fig. 8 shows how the Achilles is loaded when running.
Figure 8. Running puts far more stress on the Achilles than walking. The Achilles is under tension from first contact to heel off while the contracted calf muscles don’t change length. This is unlike walking, where the Achilles is only stressed during the latter half of foot contact with the ground.
The greatest stresses are associated with sprinting because of the speed involved and its forefoot striking running style. Forefoot strike running uses the Achilles more as a shock absorber than does heel strike running. However, the acceleration strain is the exactly the same. A sprint is a short event, so although stresses are high, the duration is brief. It is usually long-distance forefoot runners who are more likely to develop Achilles pathologies. However, all longer-distance running styles are more associated with Achilles issues than brief fast running events. Although Achilles pain does occur in most sports to some degree, it is calf strains that are more common in faster, shorter running activities, like sprinting, soccer, rugby, and hockey etc. See Fig. 9 for Achilles stresses during forefoot contact running.
Figure 9. In forefoot running, the Achilles is used as a powerful shock absorber of body weight impact with the knee and hip. Forefoot contact forces the ankle to rotate the heel downwards. This is limited by the triceps surae via high Achilles tensions.
All types of human locomotion require and utilise high elastic-recoil power around the ankle. Hence, the human Achilles needs to be relatively long and extremely thick to spread out stresses within it. Without a long, thick, and healthy Achilles tendon, all forms of human locomotion are dramatically impaired.
The role and anatomy of the Achilles
The Achilles provides the bulk of the elastic power around the ankle. Consider the Achilles as a powerful, stiffened spring sitting at the back of the ankle. It controls ankle motion and produces a very mechanically efficient recoil action for heel lifting. Although other muscles and their tendons also control ankle motion, the Achilles and its associated muscles dominate ankle forces. This is because of the immense thickness of the Achilles and the size of its connected muscles compared to the combined sizes of all the other ankle muscles and tendons together. Soft tissues such as ligaments, tendons, and the plantar fascia under the foot, also behave in a spring-like manner as body weight loads and then off-loads the foot. However, the Achilles provides the vast bulk of the power used to lift and accelerate the heel off the ground.
Tensioning the Achilles begins by contracting and shortening the calf muscles just before it loads with body weight. This tightens and stiffens up the spring-like properties of the Achilles ready for action. The calf muscles slow the rotation forward of body weight, by pulling backwards on the leg bones. They effectively act as a brake so that body weight moves forward in a controlled manner. The Achilles tensional forces increase rapidly as the leg rotates forward on the ankle at angles beyond 90º (the leg vertical to the foot). In flat-level walking, the ankle usually rotates into angles of extension by roughly around 10º (80º to the leg) before the heel is required to lift off the ground. At this point, the Achilles should be stiffened like a stretched strong spring. Heel lifting should be initiated by the release of the elastic recoil energy from the stretched Achilles springing back towards its original length. This occurs once body weight has moved away from the heel and over the forefoot, as shown in Fig. 10.
Figure 10. As body weight moves forward in walking, the ankle reaches an angle of 90º (A). The calf muscle shortens and tightens, tensioning the Achilles. The foot is flattening at this time, so tendons, muscles, and the fibrous plantar fascia under the foot stretch and tension too. Foot tensioning increases as the ankle bends forward, an act which strongly stretches the Achilles creating a spring-loaded ankle and foot (B). Once body weight has moved over the forefoot, the tensional forces within the Achilles overcome any force keeping the heel on the ground (C). The Achilles elastically recoils, shortening itself and the calf muscles. Tendons passing under the foot do the same, helping to spring the arch of the foot back up. The plantar fascia remains tensioned but also helps shorten the distance between the heel and the forefoot as the toe joints are used as pivot points.
Therefore, the Achilles is used to store and apply elastic power derived from two large superficial calf muscles and ankle motion. This spring-like action means that the heel can lift without the need for the calf muscles to assist.
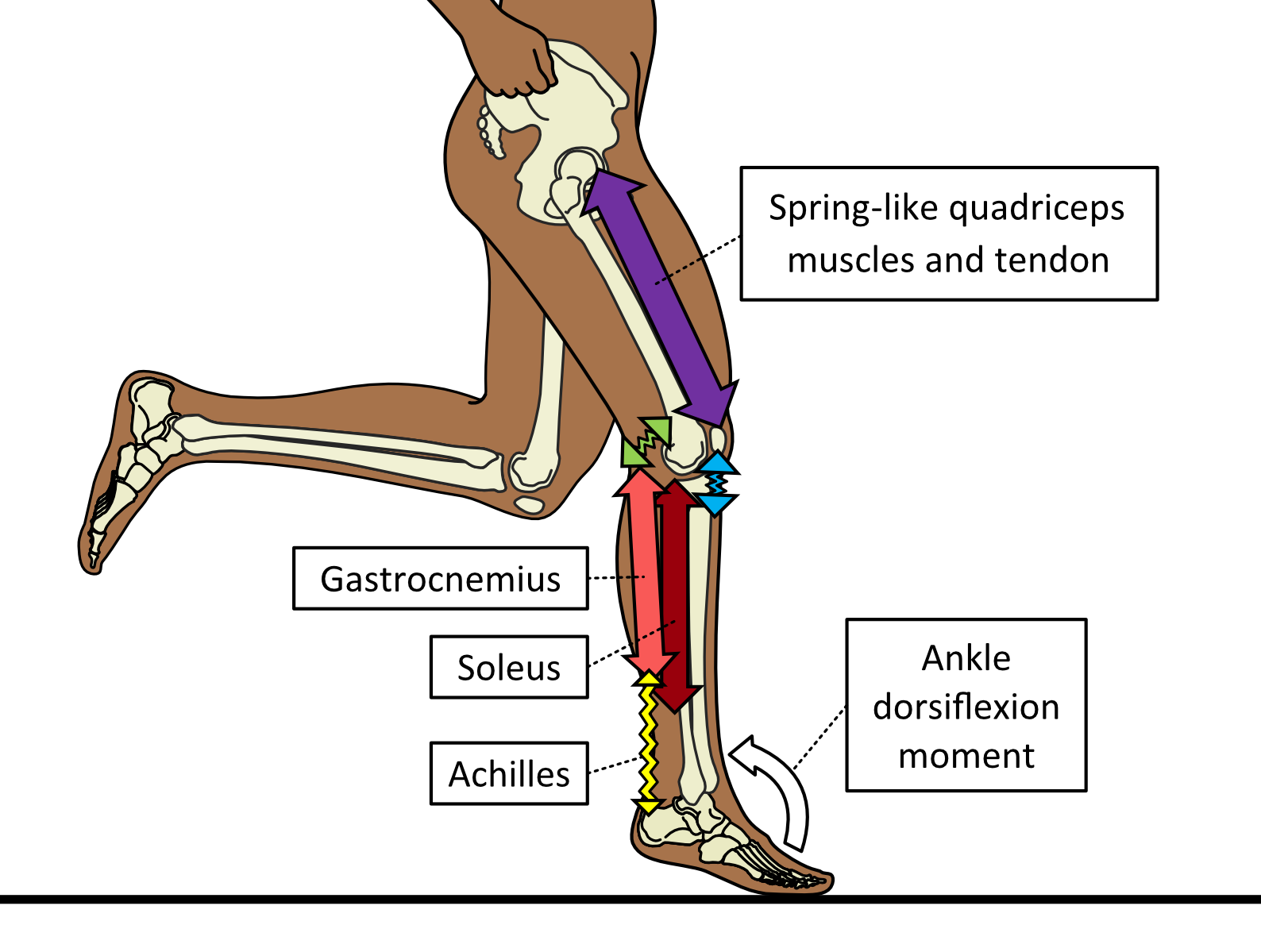
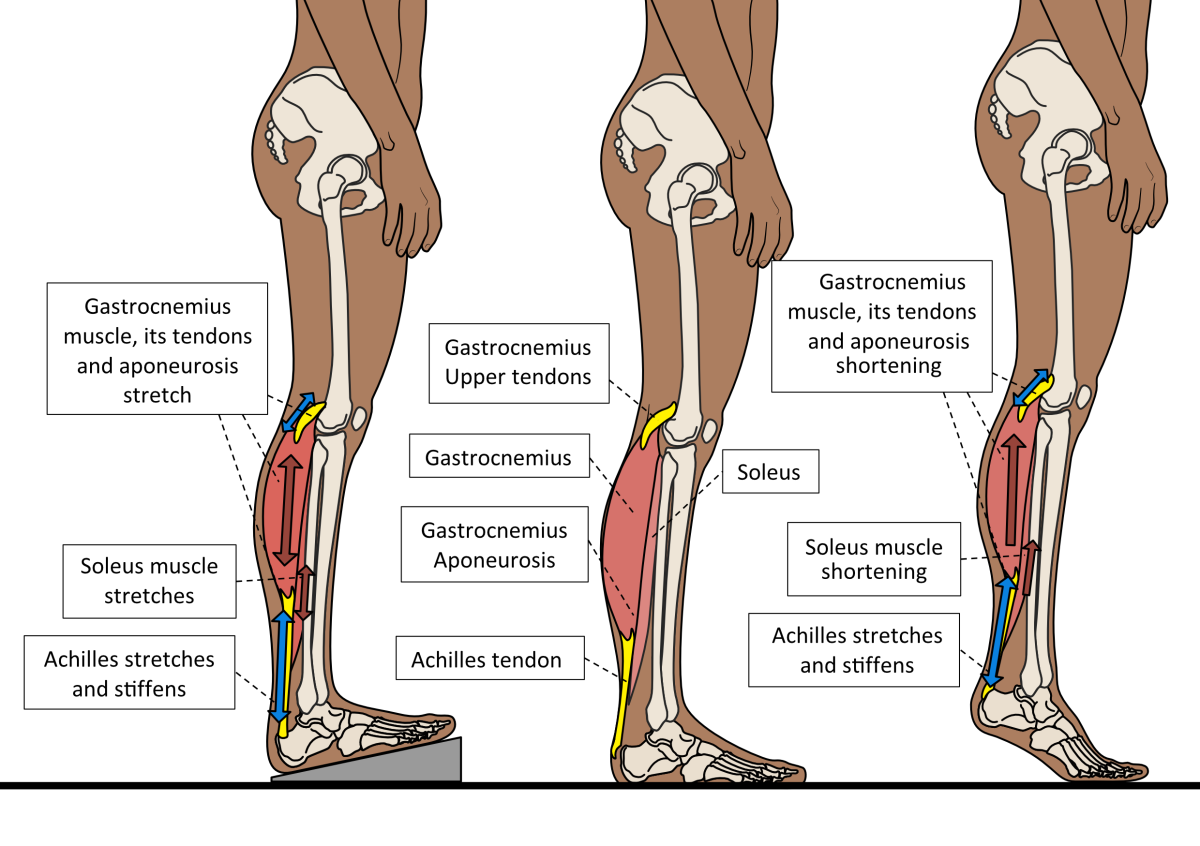
The two important Achilles-associated calf muscles are the soleus and gastrocnemius. When consider together, they are called triceps surae. They make up most of the big fleshy mass under the skin at the back of the calf. The deeper of the two muscles is soleus which lies beneath the more superficial gastrocnemius. Soleus is a large muscle that produces significant power. It primarily acts as the brake on the back of the leg bones when they rotate forward as body weight advances over the foot. It contracts relatively slowly. This makes it powerful but unable to produce sudden, explosive forces. It is the main muscle that keeps humans standing upright at rest by adding small contraction forces onto the Achilles as necessary to stop us from falling forward. The location of soleus is shown without and then with gastrocnemius in Fig 11.
Figure 11. The soleus (left) muscle lies underneath gastrocnemius (right) attached to the back of the leg bones, linked to the inner part of the Achilles tendon. Gastrocnemius is composed of two separate muscle bundles (medial and lateral), which each have a tendon attachment above the knee as well as to the Achilles.
As body weight passes in front of the ankle during walking and running, soleus activates to slow down the rate at which the leg rotates forward over the ankle. Braking body weight’s forward momentum requires strength that must be gradually applied. Suddenly ‘banging on brakes’ would ruin the smooth motion of walking and running. This explains why soleus is powerful but relatively slow contracting. Soleus uses the Achilles tendon to bridge the ankle joint, anchoring its power to the back of the heel while it pulls backwards on the leg bones (the tibia and fibula bones).
In the latter half of the foot’s weight-bearing phase, body weight falls forward under gravity and through the centrifugal forces generated by the opposite leg swinging forward. By controlling the rate of the fall, humans remain stable above a single weight-bearing limb. This is important because good stability over each single-supporting leg is essential for safe locomotion. Soleus’ power via the Achilles is essential for this. The braking power of soleus causes the Achilles to stretch and because it behaves like a spring, the power of stretch is stored as potential elastic recoil energy within the tendon fibres.
The other big calf muscle is gastrocnemius. This is found right under the skin, making up the big fleshy part in the top half of the calf, just below the knee. Gastrocnemius is divided into an inner muscle belly (medial gastrocnemius) and an outer belly (lateral gastrocnemius). Below the two gastrocnemius muscle bellies is a sheet of connective tissue that joins them together. This connective tissue sheath is also spring-like, but less stiff and more flexible than the Achilles. This is the gastrocnemius aponeurosis. This aponeurosis runs down towards the ankle to bond and form the Achilles, just where the soleus muscle also joins into the Achilles. The aponeurosis makes the upper part of the calf a more flexible area than the lower portion were soleus and the Achilles come together.
Gastrocnemius is a powerful muscle that acts more rapidly than soleus. As a result, it offers more explosive yet less sustained power. Unlike soleus, which only directly controls ankle motion, gastrocnemius also controls knee motion. This is because its two separate bellies attach via small tendons to the bottom of the thigh bone (femur), just behind and either side of the upper part of the knee.
These knee tendons are important because as body weight advances in front of both the ankle and the knee, forces want to extend the knee as well as the ankle. If this extension motion is not severely limited, the knee could be damaged. By contracting the gastrocnemius muscle to help control ankle motion, the knee receives some extension-resisting power too. This prevents the knee from extending too far, keeping it stable and safely positioned as body weight rotates forward over the ankle.
Gastrocnemius muscle power assists soleus in controlling ankle motion because it also links into the Achilles tendon. Therefore, gastrocnemius concurrently protects the knee and adds extra power into the Achilles, yet in a more rapidly changeable mechanical manner than that of the sustained power of the soleus. This gives high adaptability to the forces applied around the ankle in response to variations in walking/running speed and differences in the terrain beneath the foot. Fig. 12 demonstrates the differences in soleus and gastrocnemius control around the knee and ankle by using the Achilles tendon.
Figure 12. Once bodyweight moves in front of the ankle and knee, forces from gravity and the swing leg create forces that drive the knee and ankle to rotate into extension. By pulling on the back of the leg slowly, soleus slows the ankle’s forward rotation. This is aided by gastrocnemius which is also preventing over-extension of the knee. These actions stretch both the Achilles and gastrocnemius tendons at the knee, storing elastic power within them at the same time. The more flexible gastrocnemius aponeurosis helps protect the Achilles from the more rapid changes in gastrocnemius power.
In summary, powerful calf muscles and the Achilles work together to control ankle and knee motions when the foot is flat on the ground. This activity provides essential body and limb-stabilising forces. The Achilles is concurrently stretched and loaded with lots of energy from muscular braking of joint motion. The stored power is very important for accelerating onto the next step.
As body weight moves forward towards the forefoot, forces keeping the heel on the ground reduce to a point where the power within the Achilles is greater than the body weight forces over the rearfoot. At that moment, the elastic-recoil power within the Achilles can be released. This released power lifts the heel and flexes the knee to tip the body weight forward onto the next step. The leg swinging ahead of it now hits the ground under extra acceleration force. This acceleration force makes loading and transferring body weight to the next step much easier, vastly improving the mechanical efficiency of walking. What is perhaps surprising, is that just as we drive forward the calf muscles stop being active. They can switch off as the heel lifts because the Achilles is acting like a strong recoiling spring, doing all the work, as demonstrated in Fig. 13.
Figure 13. In the period before heel lift, the action of slowing forward momentum by gastrocnemius and soleus, loads the Achilles tendon with elastic-recoil energy as it stretches. This activity stabilises both the knee and ankle to make sure the motion at this joint is appropriate to maintain stability and prevent injury. Once body weight has moved away from the heel onto the forefoot, the elastic power of the Achilles ‘pops’ the heel up, allow the gastrocnemius knee tendons to also flex the knee. These actions together bring the swing leg to the ground.
Without a healthy spring-like Achilles, the mechanical advantage of not requiring muscle contraction at heel lift is lost. Also lost is the ability to safely control the forward motion of the body over the ankle while providing knee stability. This is why the Achilles is so important.
Achilles forces
Most muscle-generated forces pass directly through their tendons onto their bone attachment point, called the enthesis. However, some muscle force also reaches bone through the surrounding connective tissues, such as fascia and ligaments. If muscle forces did not spread out across tissues, tendon injuries would be far more common than they are.
The Achilles attaches to the heel bone (calcaneus), in an area where there is not a lot of other soft tissues to spread forces into. When forces are applied from a muscle directly through a tendon to a single point on a bone, the size of the tendon’s cross-sectional area dictates how large the attachment points must be. The Achilles attachment point is very large and nearly all forces generated by the triceps surae muscles must pass directly through it.
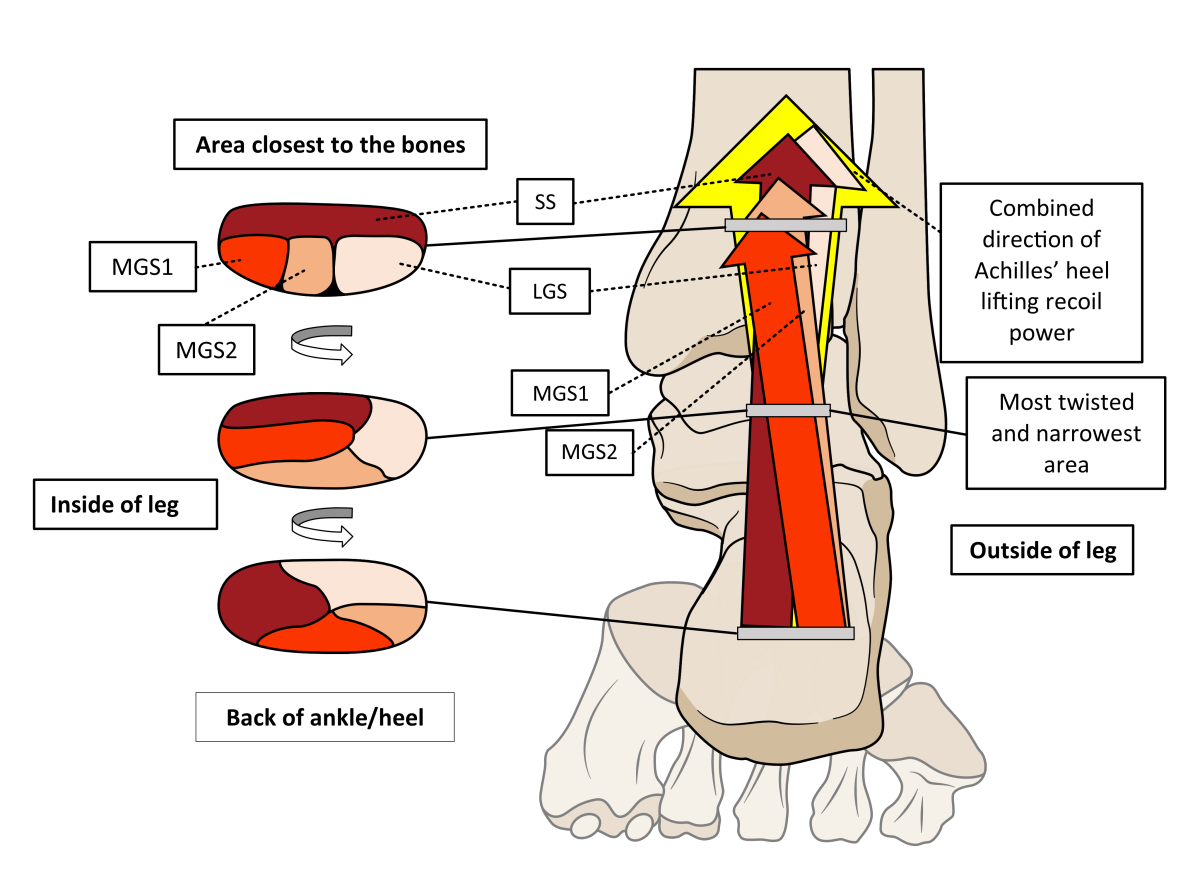
In adults, the Achilles tendon is between 4.5 to 8.5 cm wide and around 11 to 26 cm long. However, rather than being one big tendon, the Achilles is actually made up of four subtendons blended together to create a large cross-sectional area. These subtendons arise from the separate parts of the calf muscles. One arises from the soleus muscle and three from different parts of gastrocnemius. The inner or medial part of gastrocnemius has two subtendons, while the outer, lateral gastrocnemius muscle has just one. Although they all function together as one bigger unit, each separate tendon part acts slightly independently from the others, pulling on the heel bone differently. This is because they each attach to distinctly different areas of the heel bone as they gently twist together, occupying different areas of the Achilles as they descend. See Fig. 14.
Figure 14. Together, the Achilles subtendons create the power of heel lift (yellow arrow) Soleus’ subtendon (SS) starts off closest to the leg bones and slowly rotates to occupy the inner area of the attachment to the heel bone. The rotation process also gradually repositions the two medial gastrocnemius subtendons (MGS1 and 2) to the back and outside of the attachment point. The lateral gastrocnemius subtendon (LGS) ends up positioned closest to the back of the heel bone. The subtendon-twist is superb in enhancing further elastic-recoil power storage. However, it does create a thinner cross-sectional area that is vulnerable to over-strain.
Tendons are mainly made of ‘collagen’, a stiff, strong protein that forms twisted tiny microfibres and is found throughout the body. These microfibres also form twisted spirals that bind together to form thicker twisted fibres in a rope-like manner. The effect of twisting collagen fibres is much in the way that steel is not particularly elastic yet twisting rods of it can make excellent springs. When relaxed the fibres curl up, but under the slightest tension they straighten to align the fibres in the direction of tension. Tendon fibres all align in one direction so that they stretch and recoil in the same direction as their associated muscle power. See Fig. 15.
Figure 15. Tendon fibres are made of twisted collagen in a hierarchical manner, becoming increasingly elastic the more layers are added together. Thus, microfibres are more stretchy than collagen fibres, but the whole tendon is more elastic than microfibres, fibres, bundles of fibre or even subtendons.
The spring-like behaviour of tendons is perfect for assisting muscle function by reducing the chance of sudden stresses being applied to delicate muscle fibres by creating a degree of elasticity during motion. This elasticity allows joint motion, muscles, and tendons to act together as shock absorbers when moving. The only problem with tendons being built of collagen fibres, is that under certain circumstances collagen can change into something that is brittle and stiff and no longer elastic. The most common causes are diseases like diabetes and the process of ageing.
Achilles fibres all align vertically downwards from the calf muscles towards the heel bone. However, they are slightly twisted, rotating forwards towards the inside of the leg as they descend. This final twist makes the tendon behave even more spring-like. When the ankle joint bends the foot upwards (extends/dorsiflexes) to tension the Achilles, the twisting becomes more pronounced. This increases both the stiffness and the elasticity of the Achilles. Once ankle extension force is removed from the ankle, the Achilles springs back into a shortened and less twisted pre-stressed length. This extra twist is highly mechanically efficient and helps the muscles to relax at the moment of heel lift.
The amount of twist in the Achilles tendon is highly variable between individuals. This fact may be important in explaining why some people are more prone to Achilles problems than others. Although the twisting of the Achilles tendon improves its elastic power, it does create an area with a slightly narrower cross-sectional area of between 1.2 and 2.6 cm long, where the twist is most pronounced. Those with extra twisting decrease their cross-sectional area more. The narrowing of the cross-sectional area creates a slightly weaker point within the Achilles. Stress is the force over the cross-sectional area. The same force over a narrower cross-sectional area results in more stress per section of tendon.
Also by increasing the twist in the tendon as the ankle extends before heel lift, the blood vessels that supply the Achilles can be squeezed shut for a moment during each step. The more twist, the longer the loss of blood supply is likely to be. It is within this narrowest area of maximal twisting that mid-portion (non-insertional) Achilles tendinitis occurs, as shown in Fig. 16
Figure 16. The sites of Achilles tendon pathologies in relation to the subtendon arrangement and twisting. The most common mid-portion Achilles tendinitis occurs at the narrows part where the twist is most pronounced. The Achilles is wider at both its muscle-tendon (myotendinous) and bone attachment areas, where there is less twist but where different tissues meet.
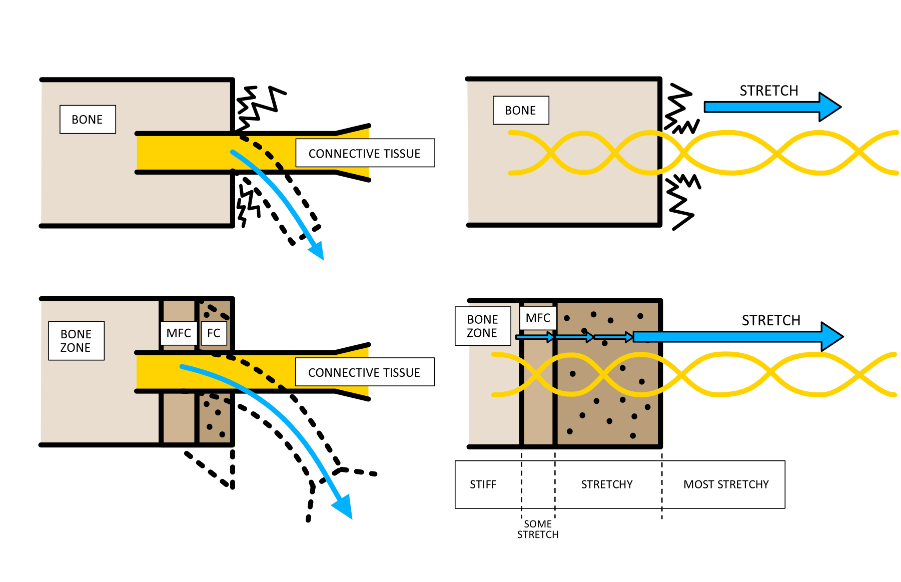
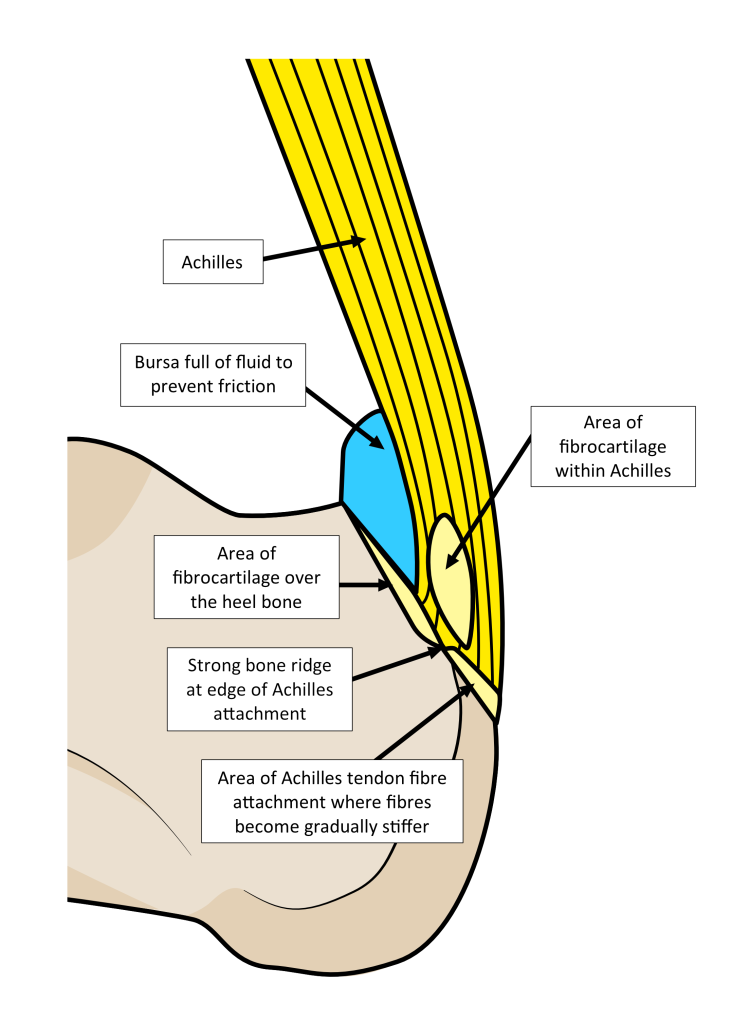
The attachment area (enthesis) is a wider, less twisted part of the Achilles tendon. This increases the cross-sectional area to help spread out forces here. Entheses are complex structures. They consist of a graduated bonding of more flexible and spring-like tendon fibres into mixed tendon and stiffer fibrocartilage fibres, and then finally blend into increasingly mineralised stiffer fibres that become bone. The gradual change in fibre stiffness prevents flexible tendon fibres bonding directly to solid inflexible bone. This avoids areas of high stress forming where material properties are dissimilar, as shown in Fig. 17. However, this graduation in material property changes can be disturbed, something we will return to later.
Figure 17. Tendons join bone through areas of mineralised fibrocartilage (MFC) and fibrocartilage (FC). The first benefit is that the greater flexibility of MFC and FC can act like the grommet on a plug, protecting the point of entry of the electric wire by allowing motion without damage. Compare upper left image without MCF and FC to the lower left image. The other benefit is that when connective tissues tension on bone, strain will not concentrate to the stiff-to-flexible interface between the bone and the stretchy tendon fibres. Compare upper right image to lower right image.
The Achilles forms a prominent bony ridge on the heel bone where it starts to attach. The fibres at the attachment have their own blood and nerve supply, making them highly active and responsive to the stresses they receive. Under increasing forces, the attachment can become stronger or else the Achilles might tear the attachment point off. Indeed, in elderly people with poor bone density associated with conditions like osteoporosis, the Achilles does sometimes pull away the posterior part of the heel bone. The injury is often mistaken for an Achilles rupture but is actually an avulsion bone fracture caused by the tensional power of the Achilles detaching weaker attachment bone.
The Achilles runs close to the back of the heel bone before it attaches onto it. To protect the Achilles from rubbing, the area above the attachment point is covered in smooth fibrocartilage with a sack of fluid (known as a bursa) lying between the tendon and the bone. Bursa can become inflamed. Bursa and fibrocartilage here reduce the risk of the tendon being over-frictioned and excessively compressed against the back of the heel bone during forward ankle rotation. In addition, the area where the Achilles is mostly likely to become compressed against the back of the heel bone has an area of fibrocartilage within it. Fibrocartilage is much better at managing compression forces than normal tendon, so by Inserting areas of fibrocartilage among tendon fibres reduces compression damage within the Achilles. However, these areas are less able to manage high tensional forces. These necessary compromises in anatomy around and at the attachment of the Achilles than can lead to insertional Achilles tendinitis, bursitis, and bone spurs, also referred to as calcification. The zones of fibrocartilage shown in Fig. 18 are the areas where bone spurs tend to form, appearing as spikes of bone on X-ray.
Figure 18. The attachment point to the heel bone (enthesis) is complex and a number of problems can arise from inflammation and degeneration.
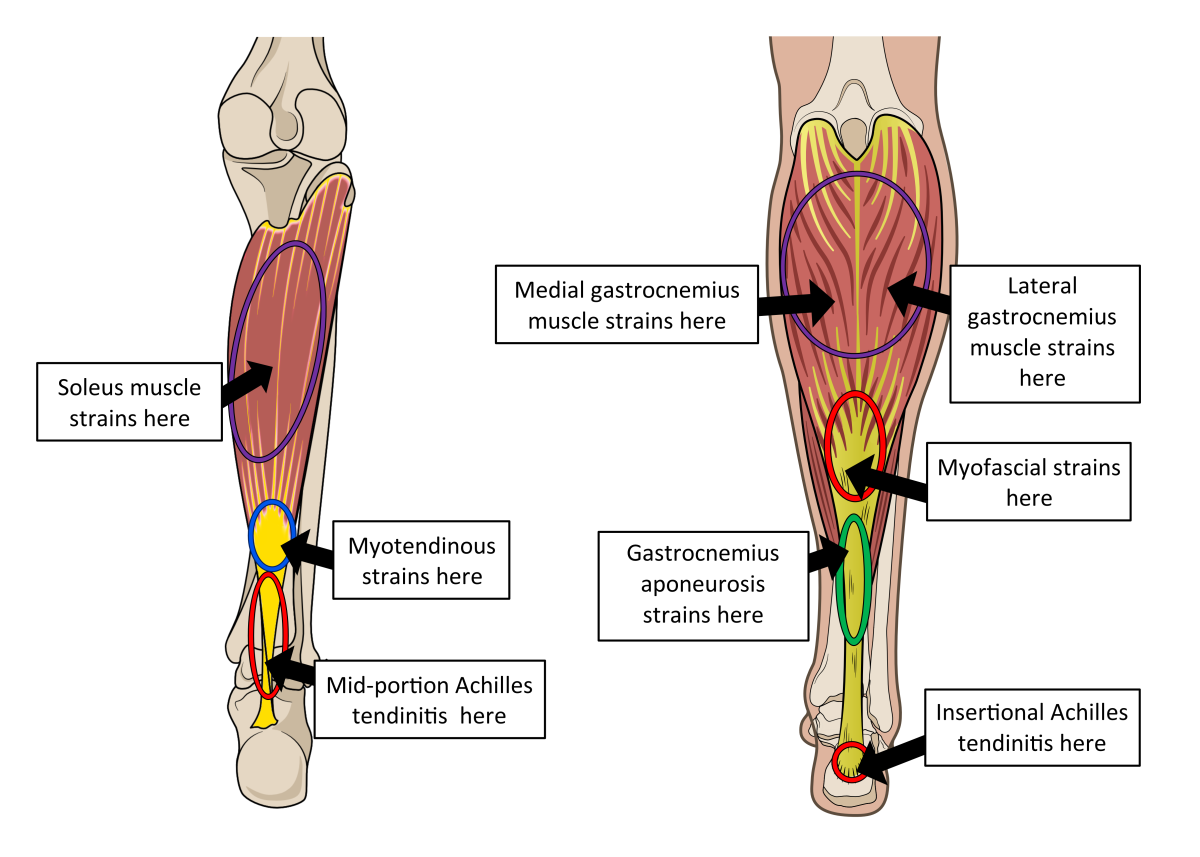
Complex anatomy is also found where the Achilles joins the soleus and gastrocnemius muscles, at myotendinous junctions. Muscle fibres actively change shape under neurological control. Muscle activity can involve them shortening (contractions), lengthening, or maintaining their length while generating stiffening force. Tendon fibres on the other hand, largely act as passive springs that change length only in response to external forces being applied through them. The joins between these different tissues are mechanically weaker areas because of their different mechanical behaviours. To spread out forces passing across the muscle-tendon interface, these joins have vast surface cross-sectional areas. The Achilles tendon is widest in its upper portion for this reason. This large contact surface area is further enhanced by using lots of microscopic undulations between tendon and muscle surfaces. Achilles myotendinous stresses are also helped by the soleus joining the Achilles lower down than gastrocnemius and by gastrocnemius joining the more flexible aponeurosis first, rather than joining to the Achilles directly.
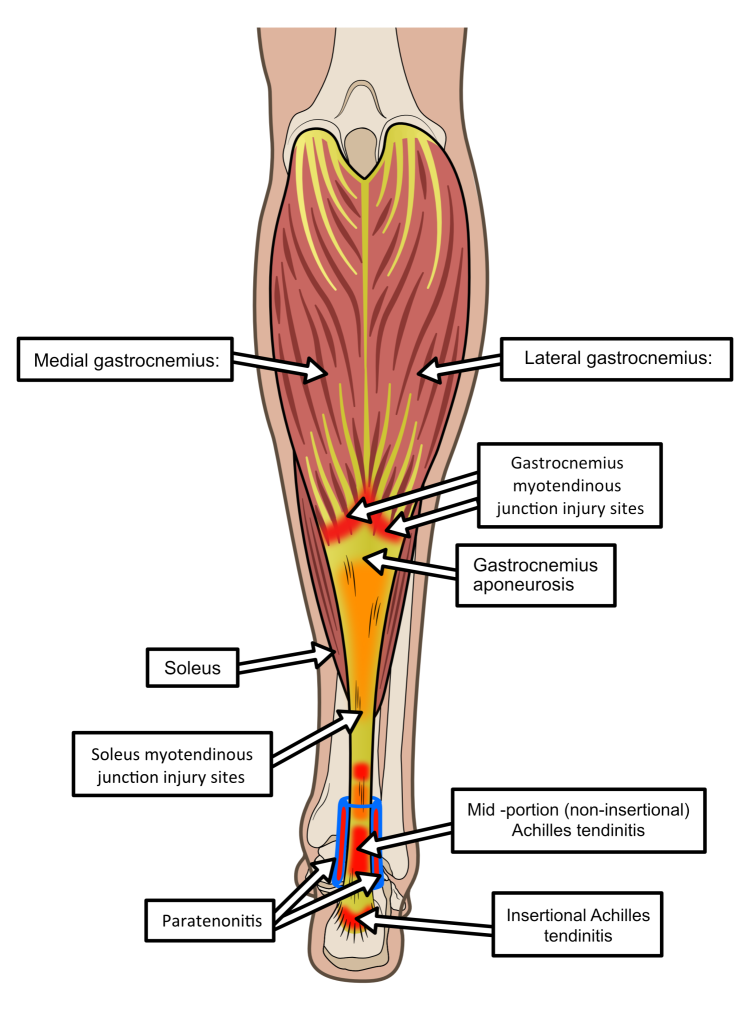
Unions between more flexible fascia and muscle (myofascial junctions) have less difference in their mechanical properties than myotendinous junctions. The aponeurosis joins the Achilles at the same level as soleus, so the Achilles has a more vulnerable connection with soleus than at the more gradual join with gastrocnemius. Graduated flexibility at the fascial-tendinous junction of the gastrocnemius aponeurosis helps reduce over-strain on the Achilles. Mechanical properties of aponeuroses are similar to those of tendons, although an aponeurosis is not as stiff. Thus, the aponeurosis can lengthen more, acting as a force-buffer between the power of gastrocnemius and the Achilles. Thus, most direct Achilles strains arise from soleus and means that myotendinous problems are more common where soleus joins. However, pathology within the gastrocnemius aponeurosis and at the gastrocnemius junction with the aponeurosis, also occur. Fig. 19 shows the locations of muscle strains, myofascial and myotendinous injuries, aponeurosis strains, and where Achilles tendinitis conditions are found.
Figure 19. The locations of calf muscle and Achilles tendon problems that all affect the ability to control ankle motion, stability, and acceleration power.
To assist power relationships between the ankle and foot, the Achilles has a very close relationship with an aponeurosis under the foot, commonly called the plantar fascia. This sits below the foot’s bones and muscles, lying just beneath the skin and directly bonded to the many foot muscles. The plantar fascia attaches to the under-surface of the heel bone that the Achilles attaches to the back of. It also binds the heel bone to the forefoot and toes, across the length and width of the arch of the foot. This arrangement links Achilles tendon forces and ankle movement to motions and strains across the foot. The presence of the tough plantar fascia helps in moderating forces between the Achilles and foot as the ankle rotates. In the young, the most posterior fibres of the Achilles run over the back of the heel bone to join the most superficial fibres of the plantar fascia. However, this continuum is lost by the end of the third decade of life. Its loss may explain the rise in both Achilles and plantar fascial problems in later adulthood. The link between fibres of the Achilles and the plantar fascia during the years when the heel bone is still growing, may explain Sever’s disease. This is a common source of heel pain in early adolescence associated with increased exercise, thought to derive from the heel bone’s growth plate mechanics. Multidirectional sports such as football (soccer), rugby, and hockey seem to be particularly linked to the condition.
Figure 20. Until full maturity (left image), there are fibres running between the Achilles tendon and plantar fascia forming a fibrous continuum over the heel bone. While the heel bone is growing, a growth plate of fibrocartilage (green area) separates the heel bone into two bone areas. Tension and compression forces on the growth plate caused by the Achilles and plantar fascia stresses during activity, help forms the best-shaped heel bone to match mechanics of each individual. Excessive stresses here provoke pain in 9 to 13-year-olds. The right image shows the mature situation, which may explain why plantar fasciitis and Achilles tendinitis are normally only seen in mature humans.
A rough guide to effective ankle and foot function
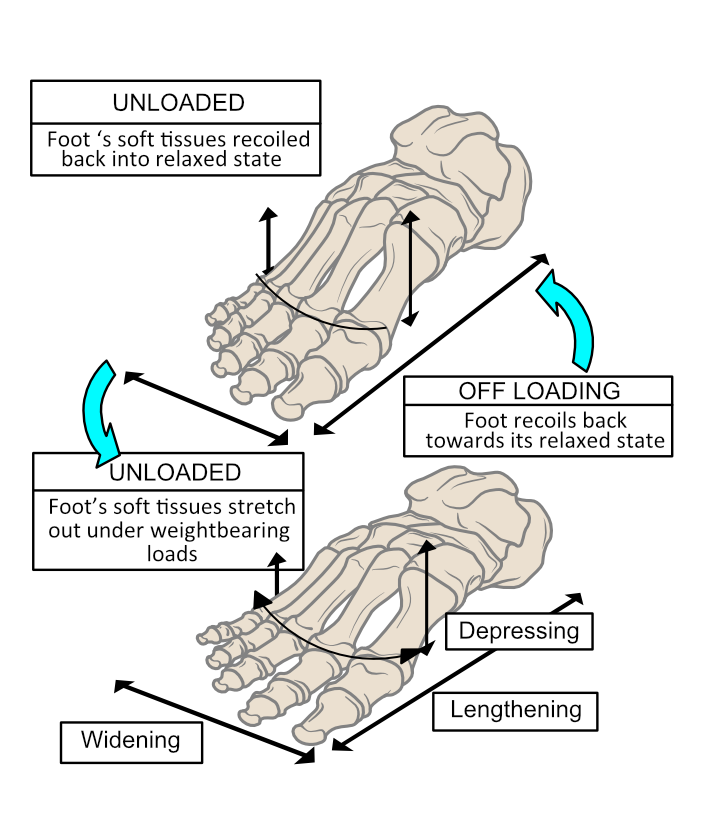
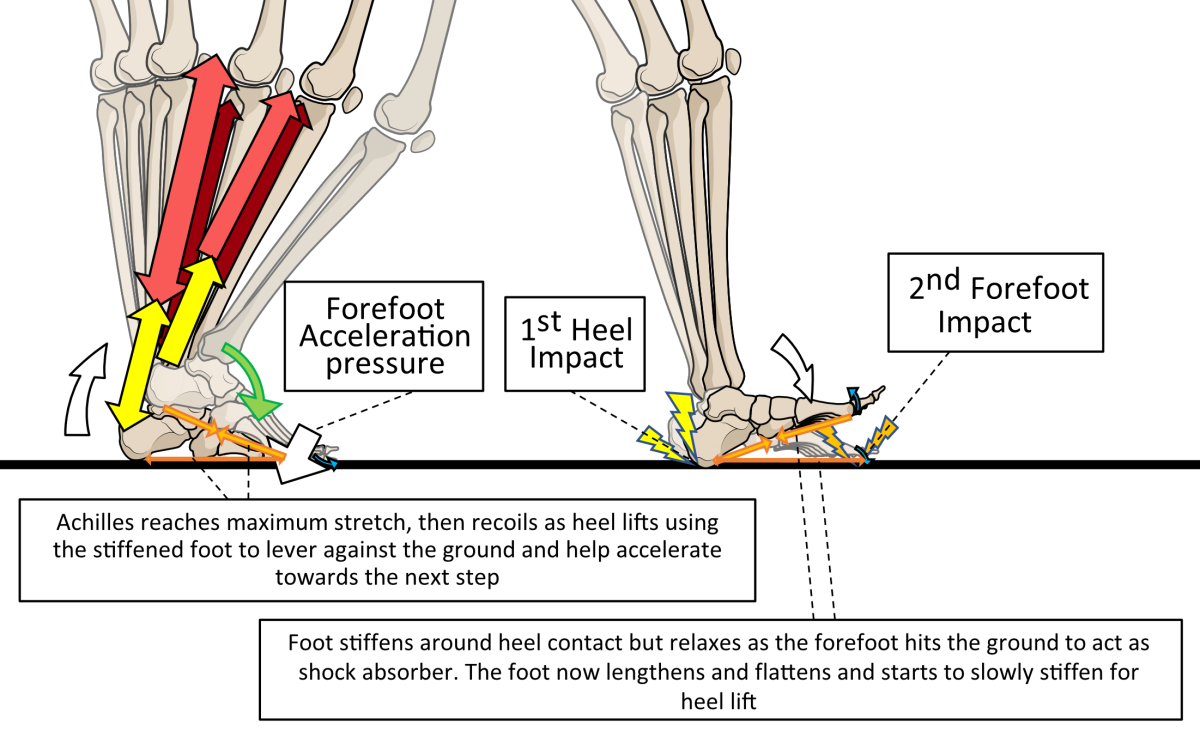
During a step, the heel usually makes first contact with the ground, followed by the forefoot after downward flexion of the ankle. This distinct two-part impact occurs partly because the foot has an arch separating the heel from the forefoot. Once the forefoot contacts the ground, all the body weight is loaded onto this foot as the opposite leg and foot start to swing forward. The foot’s arch now quickly flattens elastically to allow it to act as a shock absorber. The elastic stiffness provided by soft tissues under the foot limits the rate and amount the foot can lengthen and widen against rising tensions.
Foot flattening not only allows shock absorption, but it also increases the sole’s surface contact area with the ground. The effect of increasing surface area is to lower the peak pressures generated on the sole of the foot. Pressure is force over area. With more area in contact, forces can spread out to reduce the peak pressures on tissues under the foot. Thus, dynamic spring-loaded foot-flattening helps avoid damaging the skin and deeper tissues beneath it. As body weight unloads at the end of the weight-bearing phase as the heel lifts, the foot can spring back into shape as shown in Fig 21.
Figure 21. The foot acts as an elastic shock absorber, squashing down under load and then springing back into shape once off-loaded. Forward ankle motion that stretches the Achilles also creates forces that drives the arch of the foot downwards. This causes the soft tissues in the foot to stretch elastically. The act of heel-lifting releases elastic recoil power from both the Achilles and the foot at the same time, enhancing the spring-forward effect.
Once the forefoot is on the floor, the ankle is used rotate the body forward over the foot. The first part of this motion during walking moves body weight to a high point directly above the foot and does not use calf muscle power. However, once body weight moves in front of the ankle, calf muscles become highly active and the Achilles is tensioned. Greatest stresses are put upon the Achilles just before and at the moment the heel lifts. After this, stresses rapidly reduce as body weight is transferred to the next footstep.
The degree of forward rotation at the ankle and the amount the foot flattens have a very close relationship, so it is important to consider foot and ankle motion together. Both ankle extension rotation forward and foot flattening deformation act as shock absorbers. However, soft tissues start to act more stiffly the longer they are stretched. The foot flattens quickly after forefoot contact but as the ankle starts to rotate forward, the rate of foot flattening slows, although it still flattens. The powerful calf muscles and the slowing rate of foot flattening brakes the speed of forward acceleration while loading the Achilles with elastic-recoil power. Foot flattening in a controlled manner, helps slow the rate and the amount that the ankle rotates forward. Some braking force is applied into the foot’s ligaments, plantar fascia and foot muscles that are controlling foot-flattening. This ‘foot-squashing’ diverts some stresses into the foot’s shock-absorbing capacity and away from the Achilles and ankle joint.
Stretching ligaments, tendons, and fascia, and by also activating foot muscles, provides the foot with adjustable stiffening abilities as the ankle rotates forward. The Achilles tendon should be so full of elastic power towards the end of a footstep, that it wants to pull the heel away from the ground. This becomes an easier task as body weight moves away from the heel towards the forefoot. Lifting the heel and the middle of the foot away from the ground is much easier if the foot is semi-stiffened, so that the forefoot can then more easily push against the ground as the heel lifts. With a stiffer foot, the Achilles tendon recoil-power can lift the heel and easily rotate the ankle downwards, pivoting the foot over the big (1st), 2nd, and 3rd toe joints as shown in Fig. 22. This is the most mechanically efficient way to use the foot in locomotion.
Figure 22. After the leg has functionally lengthened through extending the hip and knee during the first part of the single limb-supporting period, the foot increasingly stiffens. Ankle rotation is slowed by calf muscle power as body weight (black spot) falls forward. This action stretches and tensions the Achilles elastically. Once body weight has moved over the forefoot, the heel ‘pops up’ off the ground under the recoil power of the Achilles. The rearfoot rotates upwards and forwards over the forefoot and toe joints, as long as the foot is stiff enough.
Thus, it is the calf and foot muscles that primarily control the rate of foot flattening and stiffening and manage the range of ankle motion used during each step. Adaptability in muscle-induced stiffness is necessary because different surfaces required different degrees of foot flexibility and amounts of ankle rotation during each step. A permanently solid or floppy foot beneath the ankle could not provide such necessary variability. Therefore, appropriate foot flattening controls pressures under it and provides stretching tensions on ligaments, tendons, and fascia, both in the foot and around the ankle. This allows the foot to act as both a shock-absorber and a recoiling spring in unison with the Achilles. Elastic power released under the foot at heel lift ‘recoils’ the foot back into shape after heel lift. Controlling stiffness across the ankle and arch appropriately avoids ligament, tendon, fascia, muscle, and joint damage that could result if the foot squashes down, or the ankle rotates too much or insufficiently.
That’s basically how a foot works with the Achilles!
Figure 23. Collision forces are applied to the forefoot of one foot under heel-lifting power arising from the Achilles (shown for the right foot), just as the opposite foot (left foot) makes initial ground contact. Achilles power adds momentum to the next step, which would otherwise be reduced by the effects of impact. By first hitting the ground via the heel and then the forefoot, the foot divides impact into two lower collision forces, rather than creating one big impact. Once the foot is flat on the ground, it continues to work as a shock absorber by flattening, lengthening, and widening. However, this process and increasing muscle activity tensions the soft tissues under the foot, stiffening it before heel lift.
What is Achilles tendinitis (or tendinopathy)?
Achilles tendinitis is a term used for Achilles pain. It means Achilles tendon inflammation. Inflammation plays only a variable role in Achilles damage and disease. Hence, all Achilles conditions tend to be referred to as Achilles tendinopathy by therapists and clinicians. It is helpful to know the precise cause of an Achilles problem to be better able to pick the best treatment options.
There are several different sources of common Achilles pains. Inflammation of the fluid-filled sleeve that surrounds the Achilles is known as paratenonitis. Inflammation of the sac of fluid near the insertion is known as retrocalcaneal bursitis. Tears can occur at the myotendinous of myofascial junction. The Achilles tendon can rupture. However, the most common problems are insertional Achilles tendinitis/tendinopathy and mid-portion Achilles tendinitis/tendinopathy.
Paratenonitis often occurs before true tendinopathy and the two conditions frequently coexists. Paratenonitis is the result of inflammation of the fibrous paratenon membrane that forms a double fluid-filled layered between the tendon and the surrounding soft tissue. The paratenon allows the Achilles to move freely behind the ankle without friction. The inner layer is attached to the outer part of the Achilles, while the outer membrane is bonded to the soft tissues that surround the Achilles. The lubrication fluid between these layers prevents friction from causing heat that could damage the Achilles during motion. However, if motion is excessive the membranes can be damaged. This results in inflammation that causes the fluid-filled space to swell and then press onto the Achilles. Inflammation therefore increases friction forces on the Achilles but in turn, previous Achilles damage can cause the paratenon to become inflamed.
Calf muscle strains and Gastrocnemius aponeurosis strain are functional problems that relate to the role of the Achilles, but they are not Achilles injuries in themselves. These are problems found higher up within the fleshier parts of the leg. Achilles myotendinous injuries usually involve muscle and tendon fibre tears along the interface between the soleus muscle tissue and Achilles. They require both muscle and tendon healing. However, many of the treatments used for Achilles tendinitis can also help calf muscle strains and myotendinous injuries.
True Achilles tendon problems are considered to start below the myotendinous junction where soleus joins the aponeurosis, just where the proper cord-like Achilles tendon starts.
Ruptures and partial ruptures of the Achilles tend to associate with sudden and brief pain. They are associated with sudden weakness at the ankle rather than Achilles pain. They usually occur where the tendon is narrowest.
The most common Achilles tendinitis is the non-insertional or mid-portion tendinitis in the middle area of the tendon. They usually associated with sport, particularly long-distance running. The damage here is caused by a combination of low-grade inflammation, degeneration, and disorganisation of the tendon fibres in the part where the cross-sectional area is reduced by the subtendons twisting. This area is also exposed to brief periods of ischaemia (cutting off the blood supply) because of the increased twisting of the tendon fibres as the ankle bends forward. This makes healing in this area particularly problematic.
Insertional Achilles tendinopathy makes up around 20% of Achilles pains. They more commonly affect daily walking activities than does mid-portion Achilles tendinitis. This pathology can cause quite significant walking-related disability. Insertional Achilles cases are sometimes referred to as an impingement (a compressive pinching) because they involve some pressure between the heel bone and the tendon, as well as tensional stresses when the ankle bends forward. The condition causes pain and thickening of the tendon around the attachment due to inflammation and degeneration close to the heel bone. The fact that these areas have significant amounts of fibrocartilage within them often encourages bone formation within the tendon fibres, known as calcifications or bone spurs. Having an enlarged abnormal bone deposit in this area (known as a Haglund’s deformity) increases the risk of Achilles tendon impingement. Pain from retrocalcaneal bursitis also occurs near the attachment and commonly coexists with insertional Achilles tendinitis. Occasionally, mid-portion and insertional Achilles tendinitis occur together.
Figure 24. The sites of the different types of Achilles related pains.
Damaged tissues attempt to repair. This initiates the complex process of inflammation. Healing tissues require increased blood flow to bring in all the substances necessary to construct new tissue. The inflammation that results causes swelling (oedema) which heightens nerve sensitivity. Inflammatory fluid also contains chemicals that cause and increase pain sensitivity in the nerves found around the Achilles and paratenon. Pain sensitivity acts as a warning to get stresses off while tissues are healing. Pain in and around the Achilles seems to prevent tendon ruptures because with pain, the sufferer is reluctant to put high loads into their Achilles, altering their gait to do so. Compared to many tendons, the Achilles has relatively few nerve endings, so most pain arises from the paratenon and other surrounding tissues.
Achilles pain is often most noticeable when standing down and starting to walk. Walking itself starts to pump some inflammatory fluid away from the Achilles and paratenon which reduces the pain for a while, unless or until forces on the tendon cause further damage. Inflammation stops once the repair is made. Then slowly pain and swelling will go away as further healing processes help the tissues to remodel to improve strength. If the repair is quick, the tendon can soon start to be loaded normally again.
However, if the rate of ankle-loading forces damaging tendon fibres outstrips the rate of healing or even just matches it, a chronic cycle of degeneration and attempted healing sets up. This involves tendon becoming infiltrated with lots of new blood vessels (neovascularisation) causing long-term problems. Healthy tendon normally has very limited blood flow, mainly around its attachment points. In circumstances of neovascularisation, the tendon fibres start to lose their organisation and scar tissue forms which does not have the elasticity of healthy tendon.
Most people who seek help with their Achilles pain are caught in a cycle of chronic healing and re-damage, with the tendon starting to lose its normal mechanical properties.
What happens as a result of Achilles dysfunction?
There are a number of potential mechanical issues that result from poor Achilles function. These are different between walking and running and between different running styles, such as heel striking or forefoot running. Pain after activity is the warning that you need to take action to allow your Achilles to heal.
Most cases of Achilles pain are in runners. Forefoot runners are particularly vulnerable. This is because they use their Achilles more as shock absorbers after the forefoot hits the ground. However, in both heel strike and forefoot running, the Achilles undergoes higher strains under greater stresses for longer.
Unlike walking, the Achilles is tensioned immediately via the triceps surae muscles activating to shorten their length and elongate the Achilles fibres to increase tension with it, even before the foot contacts the ground. This makes the Achilles highly elastic for managing braking energy into readiness for releasing it for acceleration. If the Achilles is producing pain, this elastic-recoil action becomes difficult as the runner tries to avoid loading the Achilles with too much stretch. The only option is to depower and slow running pace, and to shorten running stride length or stop running altogether.
Achilles tendinitis during walking is far more serious and indicates a more degenerate and dysfunctional tendon problem. This is because the Achilles is loaded under much lower stresses walking than occur during running. In walking, Achilles stress is greatest just at the moment of heel lift, the very moment when Achilles pains are often worse. Therefore, sufferers of Achilles tendon pain during walking tend to try and limit how much the ankle bends forward before heel lift to reduce the stretch and recoil on the Achilles. However, that also reduces how much power can be released to lift the heel and push the foot against the ground.
A dysfunctional, painful Achilles during walking causes problems in controlling the body’s forward motion during the latter half of a step. The most common reaction is to shorten the stride/step length to reduce ankle motion. Sufferers also avoid pushing the forefoot firmly into the ground when the heel starts to lift. These actions limit how far the ankle can rotate forward as the body rotates over the foot, slowing walking speed. As a consequence, the foot can be forced to squash down and flatten more as the body weight moves over the forefoot with a delay in heel lift. This can cause other injuries across the foot and ankle.
Damaged Achilles lose their elasticity. As a result, instead of heel lift occurring before the opposite foot makes contact, the heel does not lift until body weight has almost all moved onto the opposite foot. This requires a shorter stride and dramatically reduces the efficiency of walking, making locomotion harder and more tiring. A similar problem is seen with weak calf muscles and in both cases, hip muscles must become more active to compensate. This can then tire and strain the hip muscles.
Why does Achilles tendinopathy and pain happen?
People of 30 to 50 years of age are most prone to Achilles pains. Most of these are recreational runners. It is slightly more common in those who perform cold weather training, probably because cold tissues tend to behave more stiffly. The reason the Achilles becomes more vulnerable with age, is that energy-storage tendons start to mechanically change. They become less elastic and stretchable than when younger. However, you are also more likely to develop problems if you are also overweight, have previously fractured your leg or if you have experienced problems with other tendons within the leg. These problems can all put extra strain on the Achilles. Having a history of alcohol addiction, frequent use of ciprofloxacin or similar antibiotics, vascular disease, and diabetes also increase Achilles tendinitis risks. These latter issues all affect the biochemistry and physiology that supports healthy tendon tissues. Changes in tendon chemistry or blood supply tend to cause the protein ‘collagen’, within tendons to become more brittle and stiffer than normal.
Therefore, two fundamental issues lie behind problems with the Achilles tendon. The first are biomechanical problems. The second is biochemical and physiological tendon changes.
Mid-portion Achilles problems are biomechanically far more common than insertional. If the biomechanical loads on the tendon or its attachment point are excessive for the tendon to cope with, it can suffer traumatic damage. More commonly, if the frequency of higher stress loading is great, over time, minor tendon fibre strains can develop into larger injuries and damage. These situations are often called ‘overuse’ injuries. Overuse issues usually link to high stresses being put on healthy tendons when the supporting calf muscle becomes fatigued. This type of biomechanical event affects the development of Achilles tendinitis in active people. They are most common in long-distance runners who are increasing their running pace, distance, and/or frequency of running. All our body tissues are built to handle the stress levels that we regularly expose our bodies to. Thus, if we start to increase our activities, we need to do so very gradually, giving time for bones and soft tissues to reorganise themselves to cope with higher stresses. If this approach is not adhered to, damage due to tissue fatigue can occur. Once injured, tendons are less mechanically strong. Continued exercise on mildly damaged tendon tissues causes further damage, even under a lower amount of stress than that of the original cause of the injury.
Biomechanical issues related to insertional Achilles pain are somewhat different. They are more commonly related to walking stresses than cases of mid-portion Achilles pain. This is because of the difference in the application of forces in the different zones of the tendon. The profile of the foot and the shape of the heel bone play a more important part in injury involving the bone attachment point. Problems can arise if the ankle has limited ability to extend forward because the foot is not able to flatten down sufficiently. Stiffer, high-arch feet naturally interfere with the ability to rotate the ankle forwards. These feet are often called cavoid feet or pes cavus. They tend to cause the posterior part of the heel bone to stick into the Achilles as the ankle attempts to bend forward. A stiff foot that will not flatten much, tends to focus stresses back onto the Achilles heel bone insertion as well as across the foot. This results in higher compression and tensional stresses on the front of the Achilles and around its bony attachment. Sometimes, such feet tend to be more unstable to the outside edge, putting more strain onto outside Achilles subtendons, focusing pains here.
Foot and ankle motions couple together. This is important in cases of weaker feet and ankles that tend to roll inwards as the heel starts to lift from the ground. Such excessive inward ankle motion coupled to excessive foot flattening motions (often called over, excessive, or hyper-pronation) disproportionately places increased tensions on the soleus subtendon of the Achilles, focusing stresses to the inside area of the Achilles. Normally, as the ankle rotates forward, the foot flattens towards the point of heel lift. Then the ankle rotates downwards after the heel lifts and the foot rotates over the toe joints, causing the foot’s profile to increase again. Ideal free and controlled ankle rotation forward reduces the need to flatten the foot as much. If excessive foot flattening occurs, it reduces the total ankle rotation required which means less tensional stress on the Achilles, but also less ability to store elastic recoil energy within the Achilles. However, restricted ankle motion increases foot flattening stresses which can end up injuring the bones, joints, and soft tissues within the foot as well as the Achilles, when trying to heel lift.
Although foot and ankle biomechanics play a part, most cases of mid-portion Achilles tendinitis related to walking tend to involve Achilles quality problems. These are tendon issues with a biochemical or physiological cause that result in reductions in tendon performance that alters biomechanics. Rather than stresses being too high or too focused into certain particular areas, problems arise because of biochemical changes in the Achilles tissues. This makes them weaker for handling normal daily stresses. These result from problems like poor blood supply or excess blood glucose, as seen in diabetes.
Sadly, to some extent, certain biochemical changes are unavoidable as we age, and as a result even older runners normally start to change their running style because their tendons become stiffer and less elastic as they age. This is expected for energy-storage tendons like the Achilles, as these are the tendons most affected by these age-related changes. However, in the worst cases of biochemical tendon degeneration, even daily activities like walking to the corner shop can produce sufficient stress to damage the Achilles. Resolving these forms of Achilles problems is much harder.
Thus, different feet and ankles do different things, creating variable stresses across the different parts of the Achilles. Older tendons and less healthy tendons are more vulnerable. All these different factors explain why treating Achilles pain can be a challenge and why some Achilles problems are more difficult to resolve than others.
Treating each type of Achilles tendinopathy
All types of Achilles pains will respond to some of the same interventions. The primary target for treatment is to reduce the total stress on the Achilles during a step.
Heel lifts have been demonstrated to reduce strains on the Achilles in cases of both mid-portion and insertional Achilles tendinitis. Those with Achilles pains who have used heel lifts in research conditions have reported reduced pain severity and improved quality of life compared to those who just used exercises in only 2 weeks. However, research also indicates clearly that rehabilitation exercises used for insertional and mid-portion Achilles pains should be a little different.
Healthy Steps X-Line AT insoles have been designed by our in-house podiatrist with consideration to all the complex factors that affect the development of different forms of Achilles tendinitis. They incorporate a heel lift and rocker to reduce Achilles stresses by aiding the action of heel lift. They also provide a specific contoured profile to stabilise the foot and ankle so that certain motions cannot detrimentally disturb Achilles function. This makes this product suitable for assisting all types of Achilles dysfunction, except a full Achilles rupture.
X-Line AT insoles are also an integral part of the Achilles Fix Kit.
The Achilles Fix Kit is the only commercially available total treatment package for Achilles tendinitis that includes not only insoles specifically designed for Achilles tendinitis, but also foot and ankle rehabilitation aids. It includes tape for immediately relieving symptoms and also compression hosiery to improve calf mechanics and help keep calf tissues warm to aid healing. There are advice sheets and additional online support. This is an ideal aid for the long-distance runner with a troublesome Achilles and/or calf muscle.
Mid-portion/non-insertional Achilles tendinitis
Key Solutions for mid-portion Achilles tendinitis:
- Strengthen the calf muscles through their full range of motion (see Fig. 25)
Figure 25. For mid-portion Achilles tendinitis, use a stretching platform for 2 minutes (left) and perform a heel dropping and raising calf exercise (right) 10 times or until pain is felt, whichever is the greater.
Strengthen the foot muscles using exercises:
Foot Rehabilitation Ball exercise
Toe motion exercise
- Use X-Line AT insoles even in the house
- Use X-Line AT insoles until symptoms have resolved for at least 6 months afterwards
- Use Achilles taping to moderate pain
- Consider shockwave therapy from a clinician/therapist if symptoms are not improving after 4 weeks treatment with the correct shoes, insoles, taping, and exercises
- If you are a runner, use trainers that have a small heel lift (significant drop) only flex easily across the base of the toe area, and are relatively light. See Fig. 26.
- These types of trainers are also a good option for those who’s Achilles tendinitis is related to walking as X-Line AT insoles easily fit inside. See Fig. 26.
Figure 26. Relatively light trainers with a heel raise built in. Make sure they only flex easily in the area shown.
Insertional Achilles Tendinitis
Key Solutions for Insertional Achilles Tendinitis:
- Strengthen the calf muscles only within the ‘plantarflexed’ (or flexed) range of ankle motion. The easiest exercise is lifting the heel from the floor and moving onto tiptoe. Then slowly lower the heel back to the floor and then repeat 10 times or until pain is felt, whichever is the greater. See Fig. 27.
- Stretch the tissues that support the calf muscles passively, ideally using a stretch platform. Controlled stretching of calf tissues will help when combined with strengthening, shown in figure 27.
Figure 27. For insertional Achilles tendinitis, use a stretching platform for 2 minutes (left) and a heel raising exercise from the flat floor to tiptoe and slowly back down again.
Foot strengthening and mobility exercises:
Foot Rehabilitation Ball exercise See above the for the video.
Toe motion exercise See above the for the video.
- Avoid flat shoes, wear shoes with 1cm+ heel raise above forefoot, even in the house.
- Use X-Line AT insoles until symptoms have resolved and for at least 6 months afterwards
- If symptoms are not improving after 4 weeks treatment with the correct shoes, insoles, taping, and exercises, consider shockwave therapy from a clinician/therapist.
- Using stable supportive shoes with some heel lift and X-Line AT insoles might prove to be essential to prevent pain from now onwards, especially when walking any distance. See Fig. 28
Figure 28. A significantly heeled boot or something similarly supportive helps avoid problems with Insertional Achilles Tendinitis in the long term, especially if feet are stiff and high arched.
Myotendinous junction injuries
Key Solutions for myotendinous junction injuries:
- Strengthen the calf muscles using exercises as in Fig. 25
- Strengthen the foot muscles
Foot Rehabilitation Ball exercise See above the for the video.
Toe motion exercise See above the for the video.
- Use stable supportive shoes until symptoms are fully resolved, even in the house.
- Use contoured arch supportive insoles until symptoms have resolved and for at least 6 months after for exercise.
- Use taping to moderate pain in the early stages of treatment if exercising
- Consider soft tissue massage or manipulation if not resolved withing 4 weeks.
Paratenonitis
Key Solutions for paratenonitis:
- Strengthen the calf muscles using exercises in both Figs 25 and 26.
- Strengthen the foot muscles
Foot Rehabilitation Ball exercise See above the for the video.
Toe motion exercise See above the for the video.
- Use AT supportive insoles until symptoms have resolved for at least 6 months afterwards.
- Avoid thin-soled, flat, soft, and flexible shoes. Lace-up comfort styled shoes or boot with a small raise in the heel (rather than completely flat) are by far the best option, which includes trainers that only flex across the toe area see Fig. 26.
For more tips and information, go to the AchillesHub
Sources of Information
The bulk of the information provide here was sourced from the two medical textbooks. The books are extensively referenced from peer-review medical and scientific literature, and are published by Academic Press, an imprint of Elsevier.
Clinical Biomechanics in Human Locomotion: Origins and Principles.
Andrew Horwood, with contributions from Nachiappan Chockalingam
ISBN 978-0-323-85212-8
Clinical Biomechanics in Human Locomotion: Gait and Pathomechanical Principles.
Andrew Horwood, with contributions from Nachiappan Chockalingam
ISBN 978-0-443-15860-5
Both textbooks are available directly from the publisher or through other online and academic book retailers. They are written for a medical audience with some prior anatomical knowledge.