BUNIONS and HALLUX VALGUS
Bunions And Bunionettes
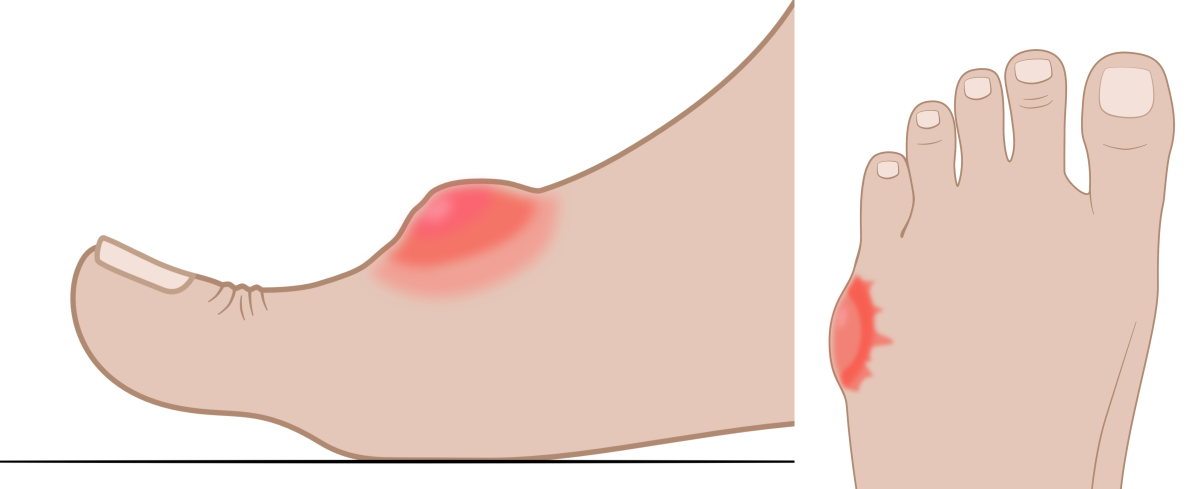
Strictly speaking, bunions are enclosed sacks of fluid lying under the skin and over part of the big toe joint. Such sacks of fluid (bursa/bursae) form to protect anatomy from rubbing pressures. Bursae can occur as part of normal development, or as a result of abnormal rubbing of anatomy later in life. Bunions are usually acquired as a result of rubbing from footwear. If the rubbing and pressure causes inflammation of this bursa (known as bursitis) the bunion can become painful.
Bunions commonly form on the side of big toe joints. This is often associated with a prominent big toe joint that rubs on footwear.
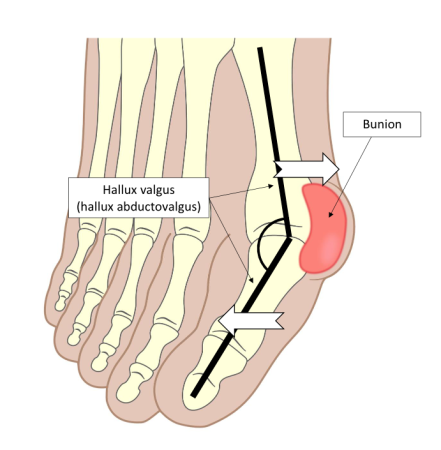
The term bunion is often erroneously used to mean a hallux valgus deformity (also more correctly known as hallux abductovalgus deformity). Hallux valgus causes the big toe joint to stick out on the inside of the foot, while the big toe itself turns outwards towards the little toe. This forms a prominent joint that footwear can rub upon to create bunions.
Hallux valgus (hallux abductovalgus) is a foot deformity that results from the big toe drifting towards the little toe, while the metatarsal bone behind it drifts inwards. This forms an angle between the toe bones and the metatarsal, creating a prominence on the inside of the foot where a bunion can form.
Bunions can also form over the top of arthritic big toe joints due to deposition of new bone around the joint’s edges, which enlarges it. Such thickened joints can then rub their overlying skin against shoes. These are called dorsal bunions. Bunions next to little toes are called bunionettes.
A bursa over the top of the big toe is known as a dorsal bunion. They often form over thickened arthritic joints. A bursa near the little toe is known as a bunionette. These can also become inflamed.
Painful bunions can be resolved by changing footwear, whereas painful big toe joints can be assisted by insoles such as the X-line DJD. Large hallux valgus deformities may require surgery.
Hallux Valgus
Hallux valgus (hallux abductovalgus) is a deformity that results from the biggest metatarsal bone (long bones across the running through the forefoot) on the inside of the forefoot drifting inwards, while the big toe moves outwards. This occurs at its joint with this metatarsal, moving the big toe towards the little toe. The reason that the deformity occurs is complex but largely relates to poor or unbalanced muscular activity around the big toe joint. Hallux valgus tends to hereditary tendencies, often occurring among family members across generations. However, it is not directly a
genetic issue.
Hallux valgus can develop in late childhood or during teenage years, but mostcommonly arises within adulthood. Very rarely it can be present at birth. When developed during childhood, hallux valgus may form as a result of joint development issues at the base of the big metatarsal and the bone behind it (the medial cuneiform bone). There is probably some degree of footwear involvement in this process. Teenage and adult forms seem to strongly link to footwear styles that compress toes together and limit their motion.
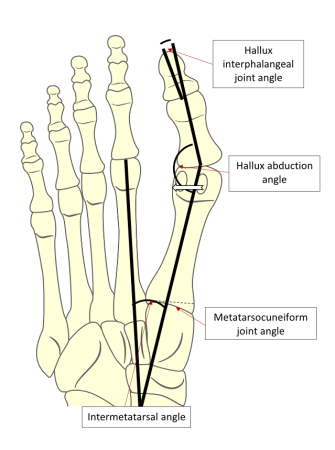
Hallux valgus deformity can occur at the big toe joint, at the joint at the base of the long metatarsal bone, and sometimes at both joints of this metatarsal. The joint within the big toe can also deform, making the big toe deviation towards the little toe look worse.
The underside view of the bones of the foot showing Hallux valgus (hallux abductovalgus). This is a deformity where the big toe rotates towards the little toe. However, the deformity can involve changes in the alignment of the toe joints (hallux interphalangeal joints), the big toe on the metatarsal (the hallux abduction angle), and between the metatarsals (the intermetatarsal angle). In some cases, the metatarsocuneiform joint excessively angles inwards compared to its more normal position (dashed line). Often the little oval bones under the big toe move out of position towards the little toe.
Without surgery, the deformity is difficult to resolve and surgical outcomes are not always satisfactory. Pain associated with hallux valgus can be aided by insoles such as the X-line standard or X-line RIF. However, providing roomy toe space within footwear is very important and that alone can keep them perfectly comfortable.
Toe Pain
Causes of toe pain are diverse.
Common causes include toenail induced injuries. The edge of one nail can cut into a neighbouring toe, or a nail can become involuted or ingrowing. An ingrowing toenail will penetrate the skin and often leads to an infection. Involuted toenails have an exaggerated curvature and pinch into the skin. Both conditions most commonly occur on the big toe, but they can also occur on others. These problems are associated with footwear use and often require surgery to cure them.
The skin of toes can also become pressured by footwear, either by directly rubbing and pressing on toes or by crushing toes together so that the areas between the toes become sore. Athlete’s foot (a fungal infection) can develop between toes causing the skin to become inflamed and split open. High pressures on toes can cause toenails to thicken or calluses and corns to form. These are common problems if toe deformities like hammer toes and hallux valgus are present.
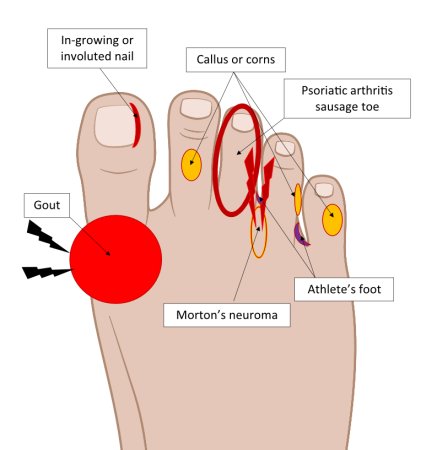 Certain arthritic conditions such as psoriatic arthritis and gout can cause painful toes. Psoriatic arthritis (often found in those with psoriasis) usually causes little toes to swell up like a sausage. Gout tends to affect the big toe and causes severe acute pain, heat, and redness around its joint. A nerve entrapment in the forefoot, known as Morton’s neuroma, can cause a radiating pain or dull ache which usually affects two of the three middle toes.
Certain arthritic conditions such as psoriatic arthritis and gout can cause painful toes. Psoriatic arthritis (often found in those with psoriasis) usually causes little toes to swell up like a sausage. Gout tends to affect the big toe and causes severe acute pain, heat, and redness around its joint. A nerve entrapment in the forefoot, known as Morton’s neuroma, can cause a radiating pain or dull ache which usually affects two of the three middle toes.
There are many causes of toe pain. Here some of the most common ones are presented.
Because toe pain has many causes, getting clinical advice via a podiatrist is advised, but a good starting point is to use footwear with plenty of toe space. Sandals can prove very helpful if enclosed footwear is part of the toe-pain problem.
Pain In The Ball Of The Foot (Metatarsalgia)
Metatarsalgia translates as pain in the metatarsals. The metatarsals are the long bones of the forefoot that run to the bases of each toe (hence there are five in each foot). These bones occupy the ball of the foot. This is an area of complex anatomy that includes skin, fatty padding, cartilage pads, muscles, and extensive joint capsule networks of ligaments and tendons, all bound together.
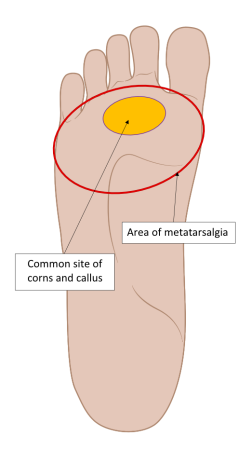
Metatarsalgia is the medical name for pain within the ball of the foot. Corns and calluses under the ball of the foot often indicate that pressures on the ball of the foot are poorly managed during walking. Commonly these hard skin lesions form in the centre of the ball of the foot. However, diffuse burning discomfort can occur anywhere within the area outlined, which is also called metatarsalgia.
There are many causes of pain within the ball of the foot because there are so many structures holding the forefoot together. Common injuries that cause metatarsalgia are joint capsule, ligament, and cartilage padding tears, tendon inflammation, muscle strains, and fatigue fracturing of the metatarsal bones. These fatigue fractures are cracks within the bones that occur under repeated loads rather than under a high force that normally breaks a bone. They are usually called stress fractures. Two little bones found in the tendons under the big toes joint called sesamoids, can also cause pain. This is known as sesamoiditis. The skin on the sole of the forefoot can develop corns or calluses that hurt, while a diffuse burning pain across the forefoot indicates that the cutaneous tissues under the skin are being sheared excessively during exercise.
Treatment will depend on the cause, but insoles, foot exercises, and footwear changes may be required.
Morton’s Neuroma
Morton’s neuroma is a swelling around a nerve in the forefoot. It is caused by a soft tissue entrapment of a nerve that supplies the underside of the little toes. Once irritated, the nerve creates sensations of toe numbness, aching, and/or pain that radiates into the affected toes. Most commonly affected are combinations of two of the middle three toes (2 nd and 3 rd toes or 3 rd and 4 th toes). The reason for this is that each nerve vulnerable to entrapped supplies the opposite sides of two toes.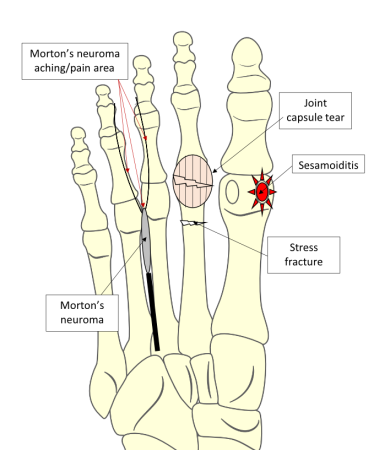
Morton’s neuroma seems to result from wearing tight fitting footwear or shoes that curve inwards (in-flared). High-heeled shoes make matters worse. Avoiding such shoes can often resolve problems in the early stages. Exercises that strengthen toes can also prove helpful. Insoles with metatarsal support that take up minimal shoe space, such as the 9-5 Everyday insole.
In more persistent cases, a steroid injection may be required to settle the nerve down. If shoe changes, exercises, insoles, and steroid injections fail to help, the nerve and its swelling may need surgical excision. Unfortunately, this leaves some permanent numbness and occasionally there are problems calming the foot down after surgery.
The underside view of the bones in the ball of the foot shows that deeper injuries can cause pain (metatarsalgia) in the ball of the foot). Some of the most common are; stress fractures (shown affecting the 2 nd metatarsal), tears and ligament strains around the toe joints fibrous joint capsule, sesamoiditis (injury to either small bone under biggest metatarsal head) and Morton’s neuroma (a type of nerve entrapment).
These causes of metatarsalgia are all problems associated with poor spreading of forces across the forefoot. They can be provoked by sudden use of thin-soled or high-heeled shoes during periods of high weight bearing activity or via their prolonged use during daily activities. Hence metatarsalgia is far more common in women. Weak foot muscles tend to make people more vulnerable to metatarsalgia.
Footwear changes to those with plenty of toe space, cushioning soles, and low heels will help. Insoles with metatarsal support and forefoot padding, like the X-line Pressure Perfect can prove beneficial as can forefoot exercises Stress fractures will need to be rested first (around 6 weeks) before foot strengthening exercises can start.