HOW THE X-LINE DJD® WORKS COMPARED TO JOINT-STIFFENING INSOLES
OSTEOARTHRITIS OF THE BIG TOE JOINT
By Andy Horwood
Product Designer and Researcher at HealthyStep Limited
What is osteoarthritis?
Arthritis means joint inflammation and it has many causes. These include local joint trauma, infection, autoimmune diseases, and gradual degeneration through poor motion and function. Autoimmune diseases result from a faulty immune system that should normally destroy infections and cancerous cells. Instead, the cells of immunity start attacking healthy tissues that in some cases includes the tissues that support joints. Such diseases include gout, rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis, Reiter’s syndrome, reactive arthritis, and those joint pains associated with inflammatory bowel disease. Many of these conditions also present with symptoms outside of the joints as well as within and around them.
Osteoarthritis (bone-joint inflammation) is a specific form of arthritis that can affect all movable joints in the body. It is a result of the breaking down of the structures that provide the mechanical properties of joints. In most cases, it is more degenerative in nature than inflammatory. Thus, it is also (and more correctly) referred to as osteoarthrosis (bone-joint degeneration) or degenerative joint disease (DJD). DJD can result from joint damage after autoimmune diseases, infection, or that caused by trauma. However, most commonly it occurs through the gradual wearing away of the joint’s structure due to dysfunctional motion at a particular joint, such as that at the big toe (see figure 1).
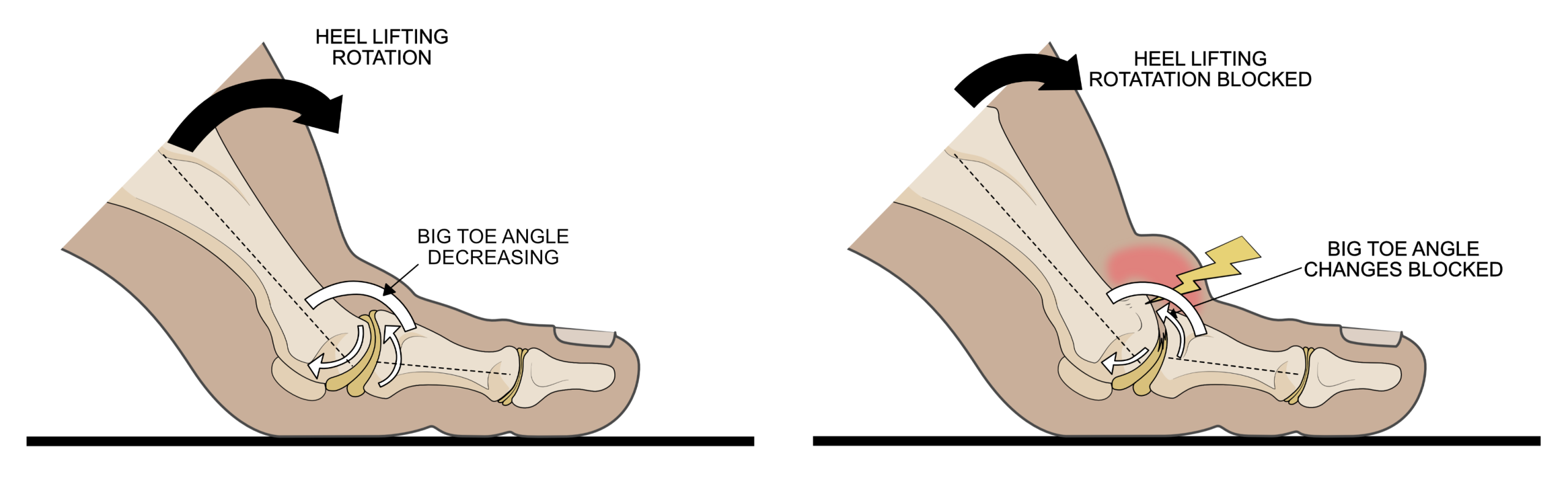
Figure 1. Healthy big toes have cartilage (beige areas within joints) full of lubricating fluid lying over well-contoured (spongy) bone. Together, these structures facilitate free motion of the foot around the big toe as the heel lifts from the ground (left image). In arthritic big toe joints (right image), the cartilage is worn allowing the joint fluid to easily flow out of the cartilage, while the bone becomes thickened and misshapen. The joint motion that normally allows foot rotation becomes blocked as the heel lifts, causing the structures around the joint to pressed together that the causes pain.
How do joints normally allow motion?
Synovial joints are the type of joint found at articulations that provide the most significant motion. Joints within the limbs, such as the hip, Knee, ankle, and those of the foot, hand, and wrist are all examples. Synovial joints consist of several important components, such as articular (or hyaline) cartilage, the ends of the articulating bone found underneath the cartilage (subchondral bone), the synovial fluid, and the tough connective tissues that form a capsule to contain the fluid within the joint. These must all be healthy for safe joint motion.
The cartilage is structed into 4 layers that are elastic, strongly compression and shear resistant, and full of fluid. The upper layer also normally offers an extremely smooth joint surface. The cartilage’s resistance to compression and shear forces are largely a result of being a structure that is full of interlinked pores that are filled with synovial fluid. Under the cartilage lies (primarily) trabecular or spongy bone which acts as a shock absorber. Between them, spongy bone, cartilage, and joint fluid provide an almost frictionless and noncompressible structure that can cope with loads many times greater than each part can in isolation. This is fortunate, as joints have to cope with extremely high forces during walking and particularly when running. During motion, such forces could easily damage cartilage or bone if it was not a ‘team effort’.
Thus, cartilage’s ability to act as a frictionless, noncompressible material is based on its structural arrangement of fluid contained within the fabric of the cartilage as well as the ability to maintain a layer of fluid between the cartilage overlying each side of the joint. The maintenance of this ‘fluid-boundary’ relies on pressures developed by the cartilage’s fluid when loaded by muscle contractions and body weight. Thus, cartilage-to-cartilage contact should not occur during motion and thereby prevent any wearing away of the tissues.
There are many special properties that cartilage, its fluid, and the spongy bone beneath offer together. These structures acting as a team offer several forms of lubrication to reduce friction on motion. These include boundary lubrication, which is the adding of a layer of lubricant across a surface. This is the effect we create when adding grease to a mechanical joint to reduce surface contact. Indeed, joint fluid is far more effective boundary lubricant than grease within a metal hinge. This is because joint fluid’s coefficient of friction is incredibly low, lower than smooth ice sliding over smooth ice. However, boundary fluid lubrication is not the primary way joints prevent frictional damage.
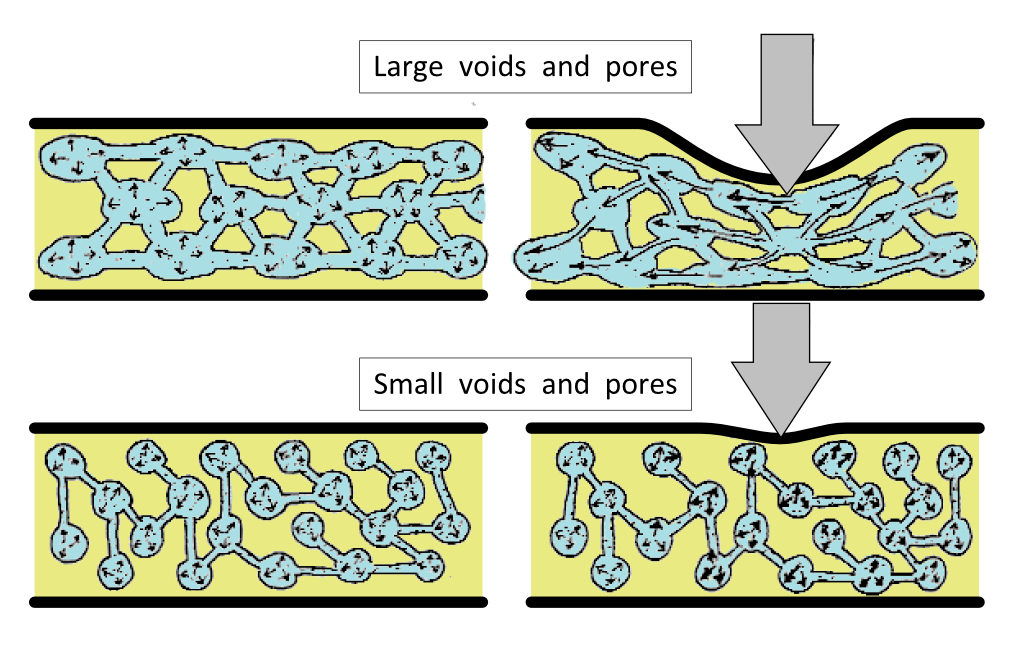
The joint fluid of lubrication also provides the cartilage tissue with nutrients to keep it healthy. To supply nutrients to all the cartilage cells, there are many millions of interconnected pores within the cartilage to permit the flow of this fluid around the joint. These interconnected, tiny fluid-filled pores provided further types of lubrication through causing internal pressurisation (hydrodynamic, elastohydrodynamic, squeeze film lubrication). When a joint moves under compression, these micropores become pressurised because the fluid within them cannot easily flow through the tiny interconnections and away from the load. Under load and motion, the cartilage is effectively ‘pumped-up’ If the pores were more openly connected, fluid would flow too easily to become pressurised to resist compression (see figure 2).
Figure 2. How well fluid is restrained in pores within the cartilage is dependent on the size of the interconnections. Larger connections between pores allows fluid to flow more easily, so that the material under load can squash down more easily (top images). Tiny interconnections make fluid flow more difficult, causing the material to act more elastically and stiffer under compression (lower images). This is a property known as poroelasticity. Healthy cartilage has tiny interconnected pores, but damaged and diseased cartilage develops larger spaces, losing its ability to resist compression by failing to create high internal pressures.
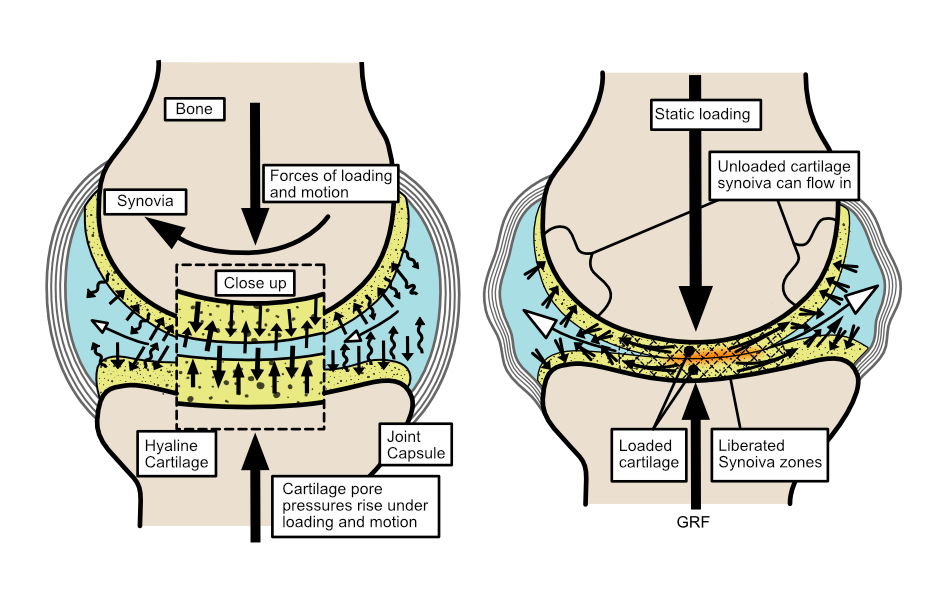
The compression on the restrained fluid causes healthy cartilage to ‘pump-up’ to resist deformation under load, while concurrently creating a layer of pressurised joint fluid that lies between the two joint surfaces. As a result of the internal fluid pressure of cartilage under load, when a joint moves the two surfaces of the joint’s cartilage should never touch. Instead, the joint creates a ‘lifting fluid force’, thereby avoiding any frictional wear.
The faster a joint loads, the greater the pressure inside the joint becomes because the fluid has little time to flow and as a result, the more the joint surfaces are kept apart. Slower loading rates causes more cartilage deformation because the fluid has more time to flow away from the compression forces. Obviously, under slower loading forces are usually lower (force = mass x acceleration). However, on static loading such as when standing, the fluid can slowly flow out of the pores and thus lose the protective fluid pressure (see figure 3).
Figure 3. Healthy hyaline (joint) cartilage uses interlinked micropores full of fluid which under compression during motion/activity, creates an incompressible, pressurised fluid-filled environment (left image). This arrangement prevents the cartilage surfaces touching across the joint (close-up in hashed area). If a joint is static for too long, the fluid within the cartilage can slowly start to flow away from compression over any longer duration (such as when standing still). This causes loss of the protective pressure, allowing the cartilage to become compressed and deformed across the joint (right image). However, if the pores become too large and freely interconnected due to cartilage damage, then protective joint pressure can be lost, even during motion.
If excessive forces are generated during an injury to a joint or disease processes weaken the structure of the cartilage, damage can occur to the walls of the pores within the cartilage. If that happens, the pores can link together to form larger spaces. Larger interconnections between pores permit more fluid flow, deflating the cartilage and allowing surface contact.
Not moving joints is a problem
When joints remain static under load for any length of time, the fluid can slowly flow between the interconnected pores and away from the compression forces towards the areas of cartilage not under load. It is a bit like taking the plug out of blow-up bed or toy, for the fluid flow between the pores occurs more rapidly at first until pressures around the joint equalises. Then flow will slow or stop as pressures lower across the joint, but the protective pressure has now been lost within the loaded area. Thus when loaded statically, joint surfaces are able to come into contact in certain places (dependent on the joint’s position at rest). When this happens, the area of the joint in contact has to rely on the mechanical elastic properties from the solid part of the cartilage, rather than the ‘lifting fluid pressure’ from the contained fluid within the pores. If this occurs within the same specific locations on a frequent basis (such as associated with a particular stance posture at work), then the cartilage in recurrent contact can start to wear away.
What happens to a joint’s function when is has arthritis/DJD
In time, splitting or tearing damage to areas of cartilage can start to compromise the whole structural properties of the joint, allowing fluid to flow more freely inside the cartilage. This is because the boundaries containing the fluid are lost, reducing the ability to create a frictionless-incompressible joint. The cartilage can now start to wear away, causing the bone underneath the cartilage to thicken, known as sclerosis. This thickening and stiffening of bone below the joint (subchondral bone) takes away the shock absorbing spongy nature of the bone that is normally found under a joint. It also deforms the normally neat contouring of the bone surfaces that oppose each other. Together, these processes increase friction and compression forces within the joint during motion, particularly around the joint edges. Cartilage doesn’t have any nerve endings, so its wear doesn’t directly cause pain. However, the tissues surrounding the joint do have lots of nerve endings and they start to produce pain on or after movement.
What happens when the big toe joint develops osteoarthritis/DJD?
The big toe (hallux) joint is a joint commonly affected by DJD. It can develop after a sudden trauma that over-loads the cartilage’s structure or more commonly, problems develop due to gradual wear and tear as a result of poor joint function during gait. When big toe joint motion starts to be affected it is often called hallux limitus. This is not the same as the clinical term ‘functional hallux limitus’, which is loss of motion during gait without a pathological (joint damage) reasons. When motion at the big toe is more severely restricted, it is often called hallux rigidus. However, where limitus stops and rigidus begins is not agreed upon by all clinicians, so they are both quite ‘loosely used’ terms.
Loss of big toe motion is a problem because it is important joint movement that is required in most footsteps to create the primary pivot-point to lift the heel from the ground. This pivot at the toes helps the body accelerate forward onto the next step. Most people will continue to drive through the big toe even with big toe joint arthritis, but after a while during (or after) exercise the toe joint will start to hurt. This often causes people to change their walking style over time, which can in turn cause problems in other joints or muscles and tendons.
Clinical Diagnosis
X-rays (radiographs) will show the extent of the disease, with MRI (magnetic resonance images) scans offering the most detail by far, including very early changes within the bone around a joint. Because cartilage is invisible on x-rays, they seem to create a space between the bones. The narrower the space, the less cartilage present in the joint. Bone appears denser (whiter) on x-ray when it is thickened, and new lumps of sclerotic bone often form around the joint edges, making the joint appear larger and misshapen. However, for treatment to start diagnostic imaging is rarely required. A good clinician can get a good idea of the extent of problem from the amount the joint has thickened on examination by palpation and how much motion has been lost on motion assessment.
Why does big toe osteoarthritis/DJD happen?
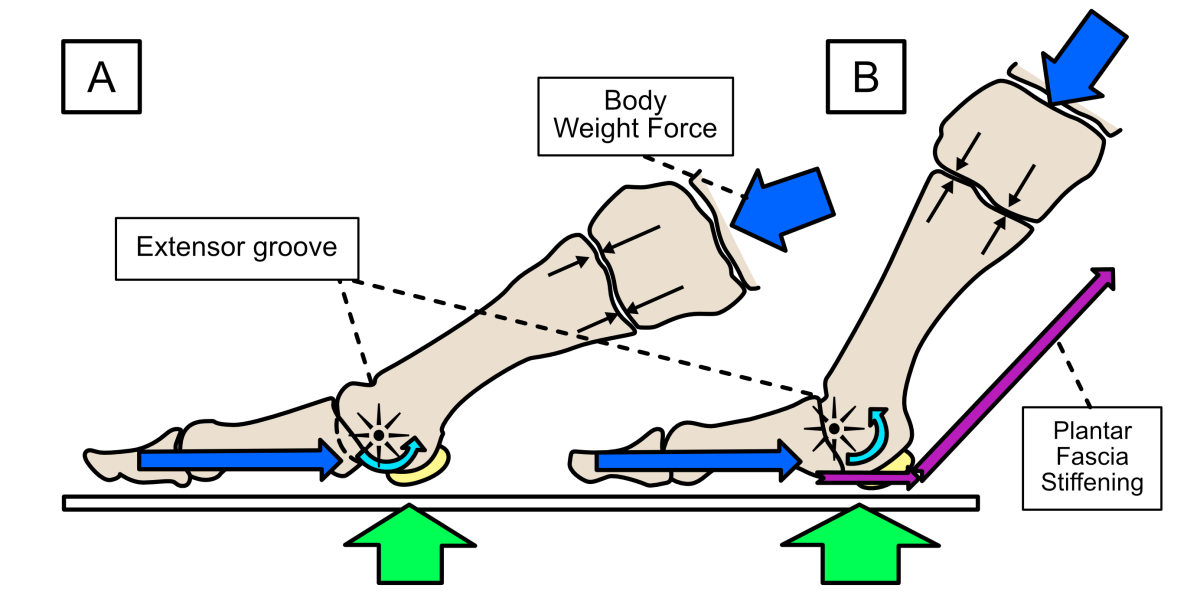
Normally the big toe rotates around the 1st metatarsal bone using a smooth arc of motion and the internal fluid pressure so as to prevent any part of the joint pinching together. There is even a little groove known as the extensor groove, that helps avoid any ‘bashing’ together of the joint surfaces towards the end of motion. The big toe joint consists of 2 toe bones, and the round head of the long metatarsal bone. The joint’s more proximal to the metatarsal bone allow some adaptability in positioning this metatarsal bone, which can glide up and down with a little side-to-side motion and rotation. As the big toe extends, an elastic/fibrous sheath (the plantar fascia) under the skin on the underside of the foot starts to tighten/stiffen, helping to stabilise the big toe and other foot joints, working with a series of muscles supplying all the toes. You can usually feel the plantar fascia under your foot when you bend your toes upwards (see figure 4).
Figure 4. A schematic of healthy big toe joint motion. Toe joint motion is controlled by muscles pulling back on the toes and body weight forces pushing forward, compressing the joint together to help pressurise the joint fluid (dark-blue arrows). Upward directed forces and pressures (green arrows) are generated under the big toe joint by muscles and body weight pushing downwards (every action has an equal yet opposite, reaction) as the foot prepares to lift the heel to accelerate forward onto the next step (A). These forces increase as the heel lifts away from the ground (B), while the metatarsal head rotates (extends) within the big toe joint, with the big toe itself held firmly against the ground.
There are two mechanisms by which big toe joints tend to become damaged as a result of the toe not rotating freely enough around the metatarsal head during the late stage of foot ground contact when walking or running.
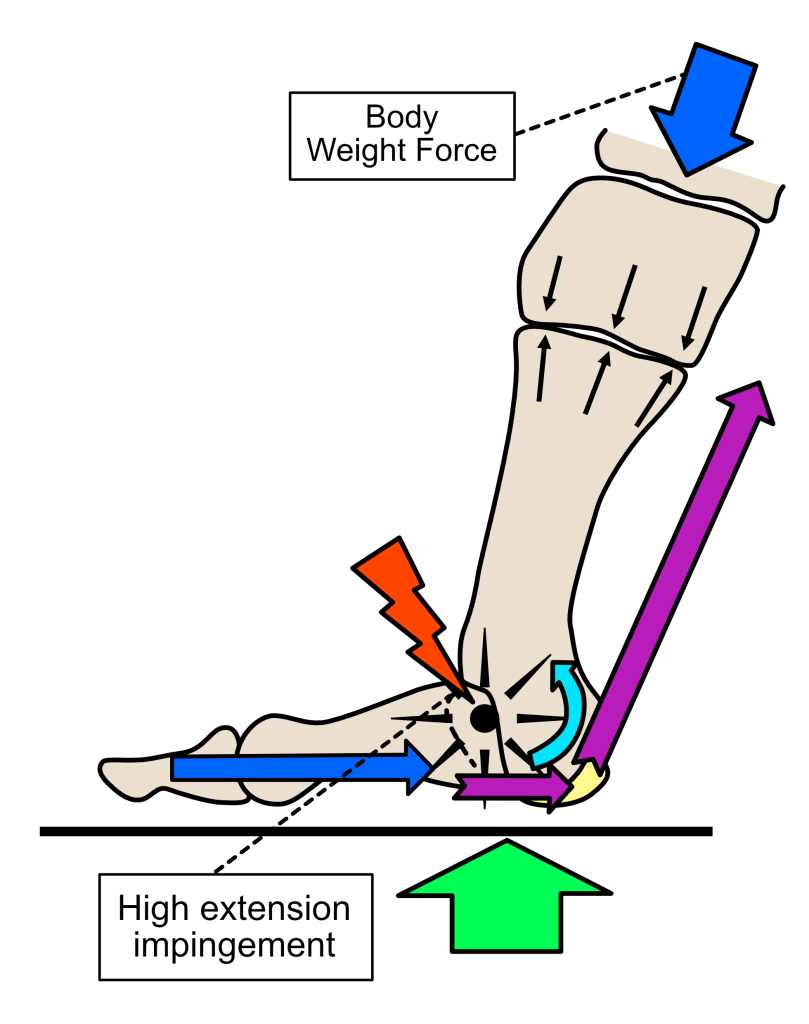
The first mechanism of damage is caused by the toe over-extending during gait (see figure 5). Most over-extension damage is gradual. This excessive toe extension can be because the toe becomes required to bend upwards more than it is shaped to do on a frequent basis. Often, this is because the flexor toe muscles that resist this extension motion are too weak to resist some of the rotation. Thus the joint does not become stable enough to rotate safely. Using heeled shoes most of the time can also demand more toe extension, which will exacerbate any muscle weakness. Most shoes have a raised heel to some degree, with higher-heeled shoes demanding larger toe extension angles. However, all shoes tend to demand greater degrees of big toe extension angles during gait when compared to barefoot. Heeled shoes will also tend to reduce the over-all range of motion of the toes used during walking. As we have pointed out, reduced motion is not good for healthy joint mechanics.
Figure 5. If the metatarsal regularly rotates into high levels of extension, the top part of the proximal toe bone risks ‘nipping’ into the cartilage on the metatarsal head, despite the extensor groove. This causes an impingement injury to the joint over time. This can damage the smooth cartilage surface and walls of the pores of the cartilage beneath.
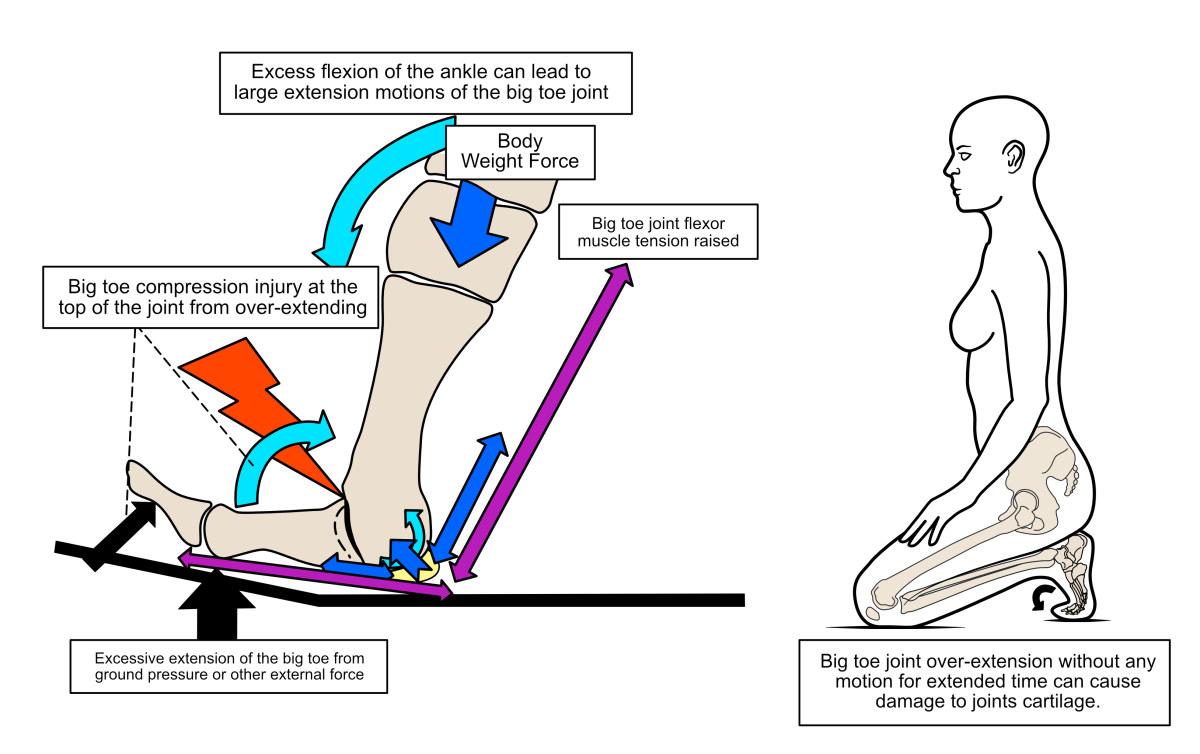
Sometimes joint extension-damage is a result of the big toe being forced by a trauma-event into an over-extension injury (known as a turf-toe injury). This causes very high pressure to occur along the top edge of the joint from the toe and 1st metatarsal bone’s head bumping together. This action impinges bone onto the cartilage’s surface, suddenly damaging it and creating a lot of pain. A risk of joint damage is also caused by long periods of sitting with the toes maximallly extended, such as when working in a squatting down position (see figure 6).
Figure 6. Sudden impacts on the big toe that drive the big toe joint into high angles of extension, can cause cartilage damage under excessive impingement forces (left image). Also, long periods of squatting with the big toe pressed into extension can also cause cartilage damage. Static loads cause problems because cartilage’s mechanical protection is limited as the joint fluid can flow out of the cartilage gradually under compression over time.
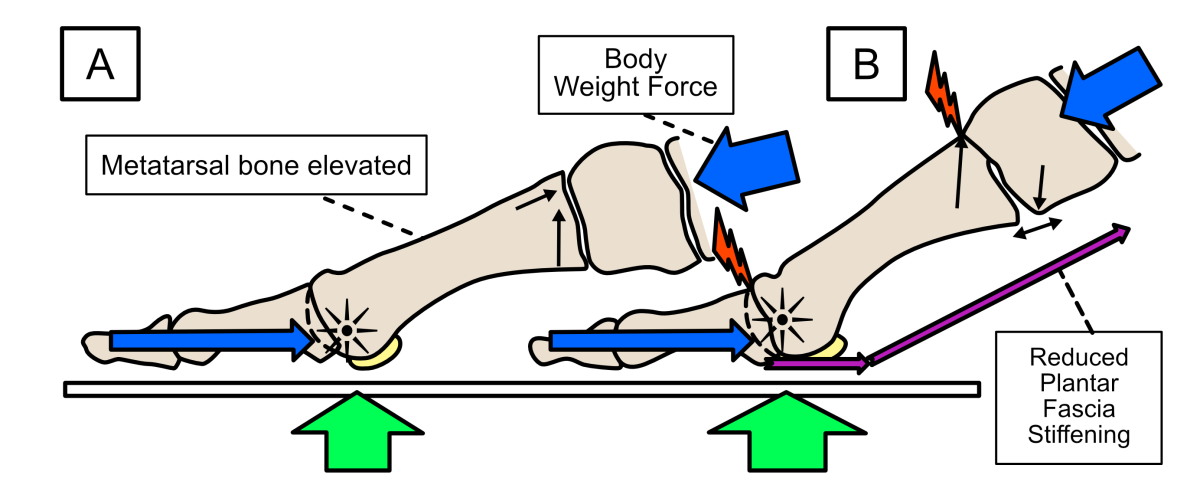
The second problem that can cause big toe joint damage, is if the metatarsal behind the toe is not firmly held against the ground as the heel lifts. This results in under-extension problem because rotating motion is not free to occur over the metatarsal head. Poor positioning of the proximal end of the big toe joint will prevent the toe from freely rotating in an arc around the metartarsal head as the heel lifts. In this situation, the metatarsal head effectively slides upwards to block the toe motion. This process will cause joint impingement on the metatarsals heads joint surface that can gradually damage the joint’s cartilage structure (see figure 7).
Figure 7. If the metatarsal bone does not position correctly before heel lift, then the rotation of the metatarsal head can become blocked. A common reason for this is that the metatarsal bone is unstable and drifts upwards when the forefoot becomes loaded during gait, becoming too elevated in its position (A). The body weight and toe-muscle forces generated now become misdirected so that the metatarsal head cannot rotate freely as the heel lifts from the ground. This can cause impingement in the big toe joint and also other joints along the inside edge of the foot (B).
Weak foot muscles and/or shoes that don’t bend across the toe joints freely enough, are often at fault in preventing the correct positioning of the metatarsals and toe joints to allow freedom of motion. However, there are many potential risks to preventing healthy big toe motion. Whatever the cause, be it acute force trauma or gradual and repeated over or under-extension of the big toe, once the structure of the solid phase of the cartilage is damaged, the fluid starts to flow too easily between pores and also out of the cartilage. Loss of normal cartilage function initiates a process of degeneration of the joint that starts to take away motion though processes of wear and tear.
What is the best treatment for big toe osteoarthritis?
Treatment should involve rehabilitation exercises for the muscles that support and provide stability to the big toe’s joint motion.
Certain footwear and the use of special insoles within them can help to reduce stresses on a damaged big toe joint during walking and running. Some insoles are designed to improve motion at the joint, but others are designed to stop motion. However, which is most likely to help in the longer term will depend on the amount of motion lost before treatment starts. Maintaining some motion is likely to preserve the cartilage for longer. Rocker-soled shoes can be particularly helpful (see figure 8 and 9).
Figure 8. There are many makes of rocker-soled shoes widely available. The key feature is a convex sole, which is stiff across the toe area.
Figure 9. A rocker soles shoe can be used to assist the heel lifting from the ground at the end of the single-support or stance phase of walking, without requiring much change in either the ankle or big toe angle. By using such shoes to roll forward, less extension range of motion of the toes is required. However, by using an X-Line DJD® inside this type of shoe joint pain can be reduced further and some safe big toe motion maintained.
Maintain motion in early stages of degeneration:
Trying to improve muscle strength and joint mobility is the best option if joint damage is mild. This is because as long at the cartilage still has functional pores to contain fluid, it has a better chance to reduce joint friction and compression forces through types of hydrodynamic lubrication. Lubrication that results from motion is far better at protecting the joint than static boundary lubrication, which still tends to permit cartilage deformation under loading. If caught early enough, healing of the cartilage damage can also occur to some variable extent. The amount of healing will depend on how early treatment starts and how much motion can be maintained.
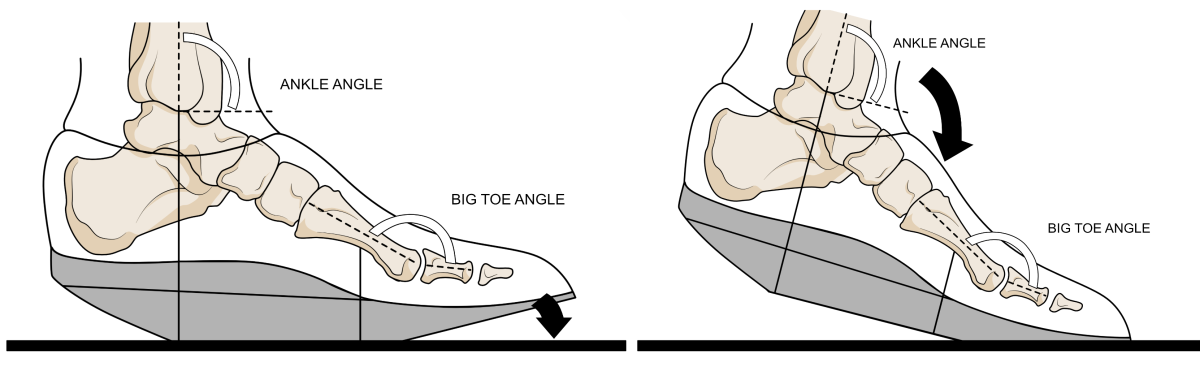
Insoles, such as the X-Line DJD® allows the joint to start its movement from a more flexed toe position. By starting in a more flexed position, the risk of over-extending the joint into impingement can be reduced. Increased motion from a flexed position allows hydrodynamic lubrication to occur where the cartilage may still be in good functional condition and reduces the chance of high loading forces occurring where that cartilage is already worn. The X-line DJD® also moves extension forces more towards the lesser toe joints and away from the big toe to help reduce stresses on the big toe joint. This is achieved by using a platform under the lesser toe joints and a downward slope towards the end of the big toe (known as a hallux trench). The X-Line DJD® also has a rocker-effect built into the forefoot area so that the toes will still move, but only into lower extension angles, hopefully keeping clear of any joint damage (see figure 10).
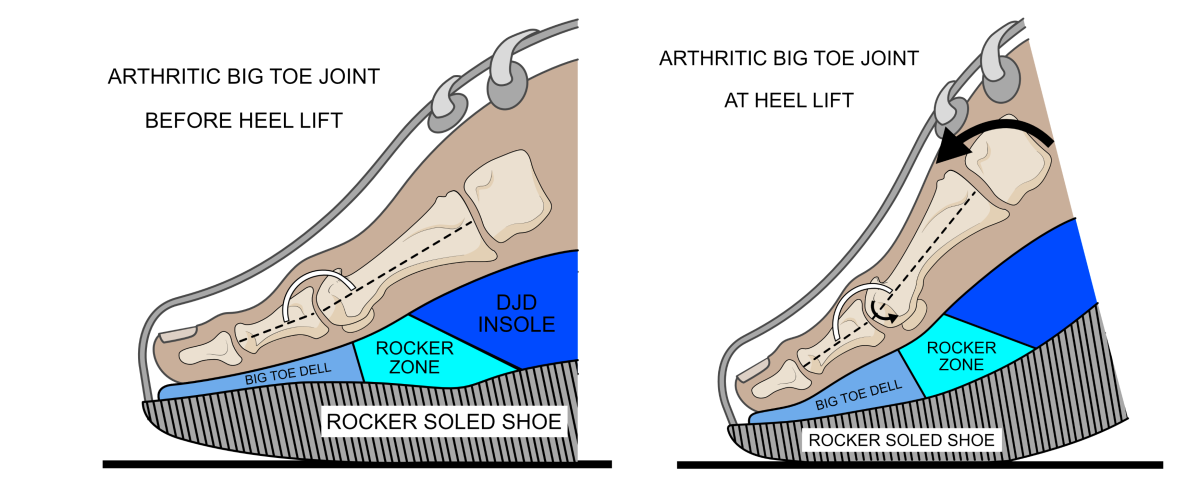
Figure 10. The DJD® insole shown working in a rocker-soled shoe. Before heel lift, the big toe joint is positioned in a less extended position via a dell formed in the forefoot of this foot orthosis (left image). At heel lift, the big toe extends as the foot rotates around the arthritic joint, but it should not move into higher angles of extension as the insole and shoe act together to pivot the foot forward. High compression forces towards the top of the joint should be avoid using the DJD®, while maintaining motion should permit some healthy cartilage function.
Shoes with a stiffer up-ward angled sole or ‘rocker-sole’ may also prove very useful when using a X-line DJD® insole by enhancing this insole’s effect. Finally, the X-Line DJD® helps encourage the correct positioning of all the metatarsals before heel lift.
Good insoles designed for big toe osteoarthritis usually require shoes with lots of space, and the X-Line DJD® is no different. Ideally, suitable footwear should have a removable in-sock that can be taken out of the shoe to create more space for a supportive X-Line DJD®. Walking boots and stiffer-soled trainers and comfort shoes are usually ideal for accommodating the X-Line DJD ®and getting the maximum benefit from it. Alternatively, certain running shoes with a carbon fibre stiffening plates inside are also benificial. This is a feature that limits how far the big toe can bend upwards, helping to prevent further impingement. They can be used for walking as well as running.
Blocking big toe motion:
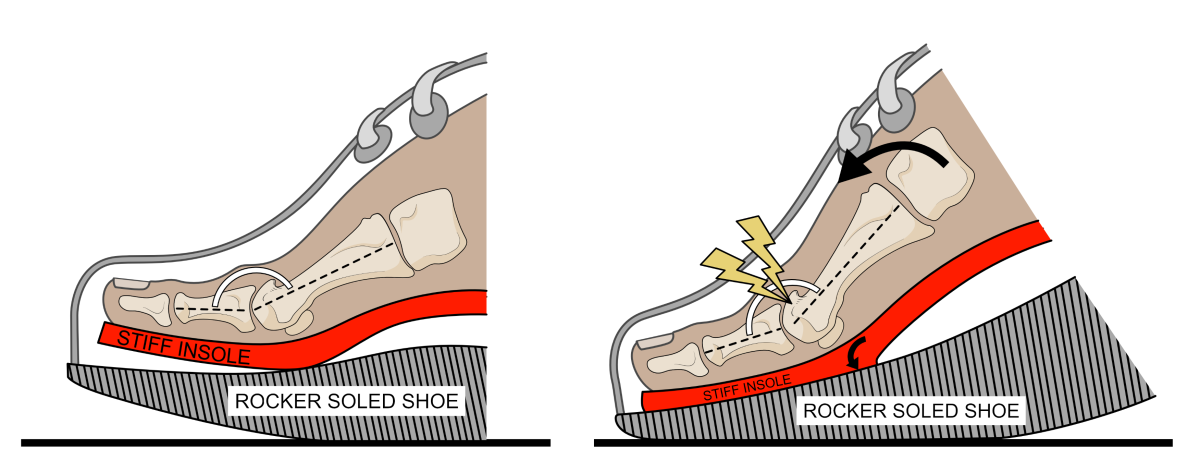
Only if the big toe joint has lost its ability to offer any significant hydrodynamic lubrication should attempting to block all motion be used. This can be attempted by using an insole with a stiffened area under the big toe joint. In severe cases of degeneration and pain, fusing the joint in a slightly upwards or extended (dorsiflexed) angled might be required to resolve any pain. Both surgery and the use of very stiff insoles means the foot will have to start to move quite differently from now on. In these cases, a ‘rocker-soled’ shoe will prove helpful (see figure11). However, if possible these treatments should onlu be used as a last resort.
Figure 11. When a joint is very badly affected with arthritis, having an insole that stops all big toe motion is acceptable, but they are better avoided in those joints that still have good motion. Shown here within a rocker-soled shoe, most are designed the hold the toe in a slightly extended position (left image). Because of the angulation under the big toe which found in many of these stiff insoles, on heel lift both the insole and the rocker-soled shoe pivot which should stop any joint motion. However, this approach does not permit safe motion that could help maintain the remaining cartilage and improve joint mechanics, but may instead risk causing accelerated cartilage destruction though stopping motion.
In summary
Where possible, it is better to regain or preserve joint motion because cartilage offers better lubrication properties when under motion than when held stiffly. Joint fluid also provides nutrients by flowing through the cartilage. This flow of lubrication is necessary to encourage any healing and maintain cartilage health. If motion is stopped or severely limited too early, the rate of degeneration may increase at a faster rate than it would otherwise. However, cartilage’s ability to heal isl very limited.
Sources of Information
The information provide here was sourced from the two medical textbooks written by the author of this article. Both books are extensively referenced from peer review medical and scientific literature.
Clinical Biomechanics in Human Locomotion: Origins and Principles.
Andrew Horwood, with contributions from Nachiappan Chockalingam
ISBN 978-0-323-85212-8
Clinical Biomechanics in Human Locomotion: Gait and Pathomechanical Principles.
Andrew Horwood, with contributions from Nachiappan Chockalingam
ISBN 978-0-443-15860-5
Both textbooks are published by Academic Press, an imprint of Elsevier. There are available directly from the publisher or through other online book retailers. They can also be ordered through your local academic book retailer. They are written for a medical audience with some prior anatomical knowledge.