Tibialis Posterior Dysfunction (TPD) is a Pain in the ‘Ankle’ and ‘Arch’!
Some muscles and tendons are well known such as hamstrings, calf muscles, or the Achilles tendon.
However, many other lesser-known muscles are at work in keeping us moving with an upright posture. They generally tend to only be of interest when they become injured.
Tibialis posterior is one of these muscles that are incredibly important for stable walking and running. When it goes wrong it is a serious problem!
Introduction
Tibialis posterior dysfunction (TPD) is a relatively common and potentially serious muscle/tendon injury located on the inside of the ankle and the inner edge of the arch of the foot.
The tibialis posterior muscle controls motion and stability across the foot and helps in stabilising the inside of the ankle. Loss of the function of this muscle is a disabling condition that causes the development of flat, weak feet and an unstable ankle that rolls inwards.
TPD is associated with damage to tibialis posterior’s tendon or within a ligament found lower down on the inner edge of the ‘arch’ of the foot. This is the plantar calcaneonavicular ligament, commonly called the spring ligament.
In America, tibialis posterior is called the posterior tibial muscle which can cause a little confusion. Many British podiatrists are now tending to use this term, referring to the dysfunctional muscle condition as posterior tibial tendon dysfunction (PTTD). However, TPD and PTTD are the same condition.
Where is the tibialis posterior muscle and why is it important?
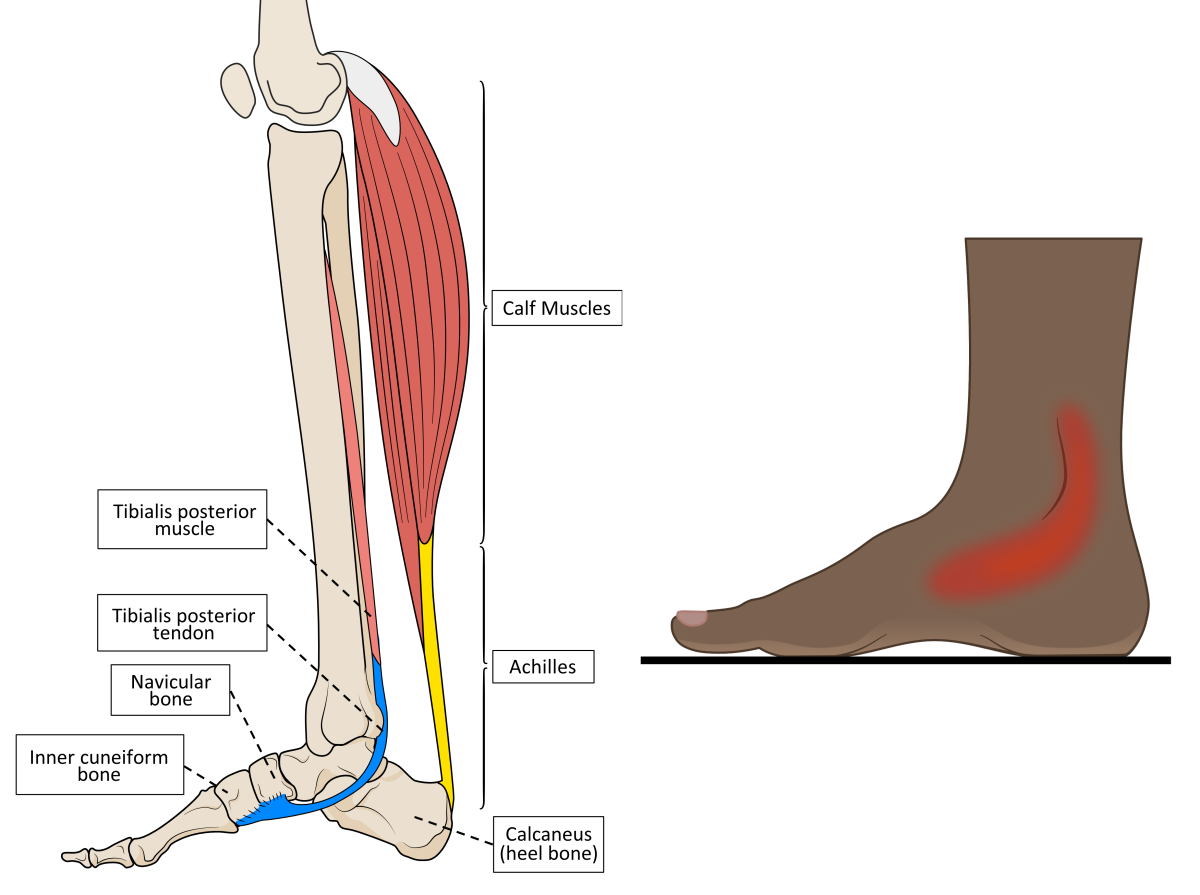
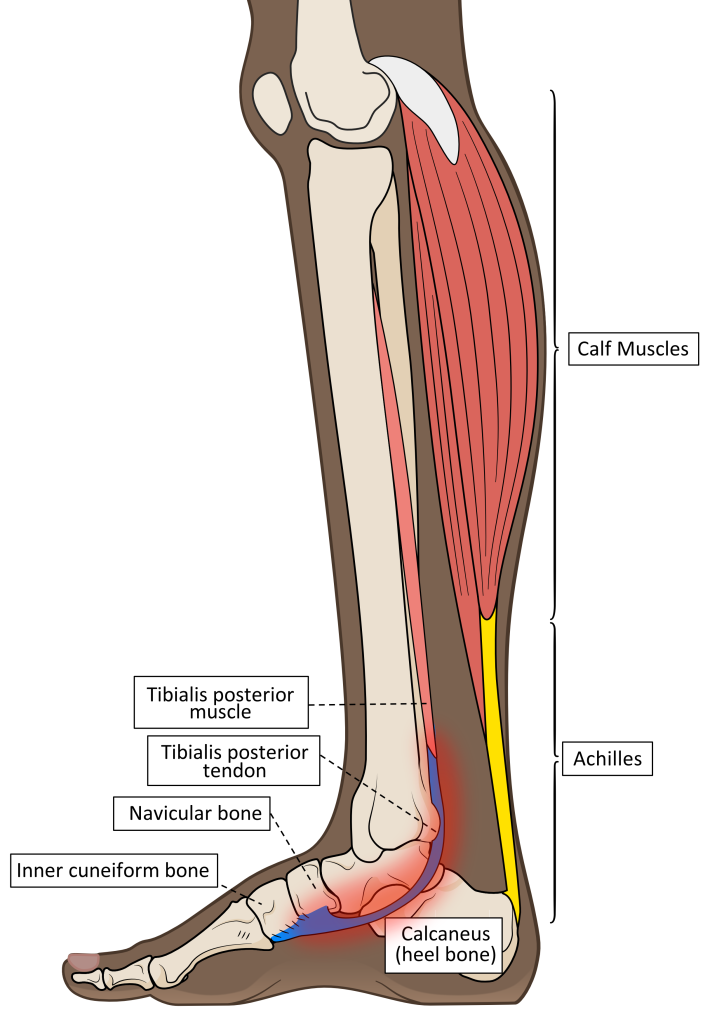
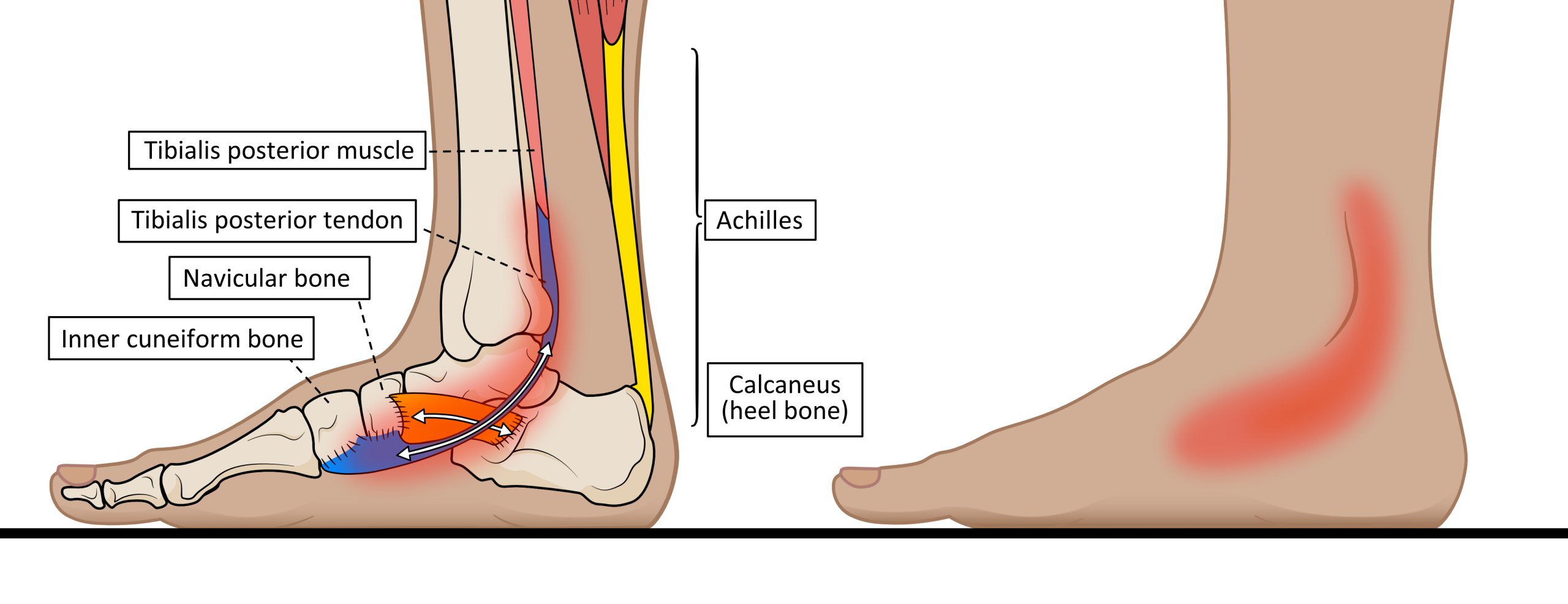
Tibialis posterior is found deep within the calf muscles, up against the back of the leg bones below the knee and passing around the ankle. The inner ankle and foot arch are the areas where pain develops in TPD, as shown in figure 1.
Figure 1. The anatomy of tibialis posterior and the location of pain associated with TPD.
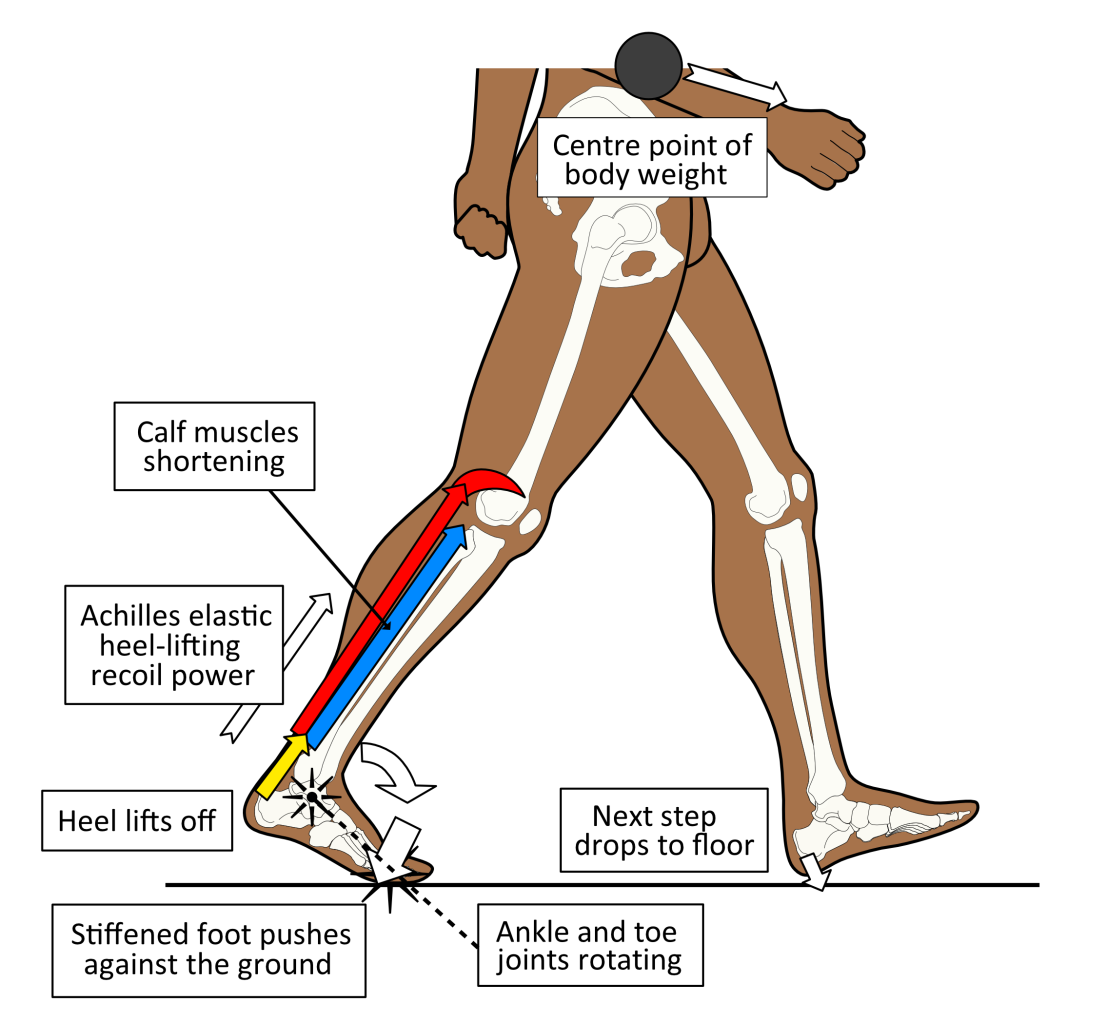
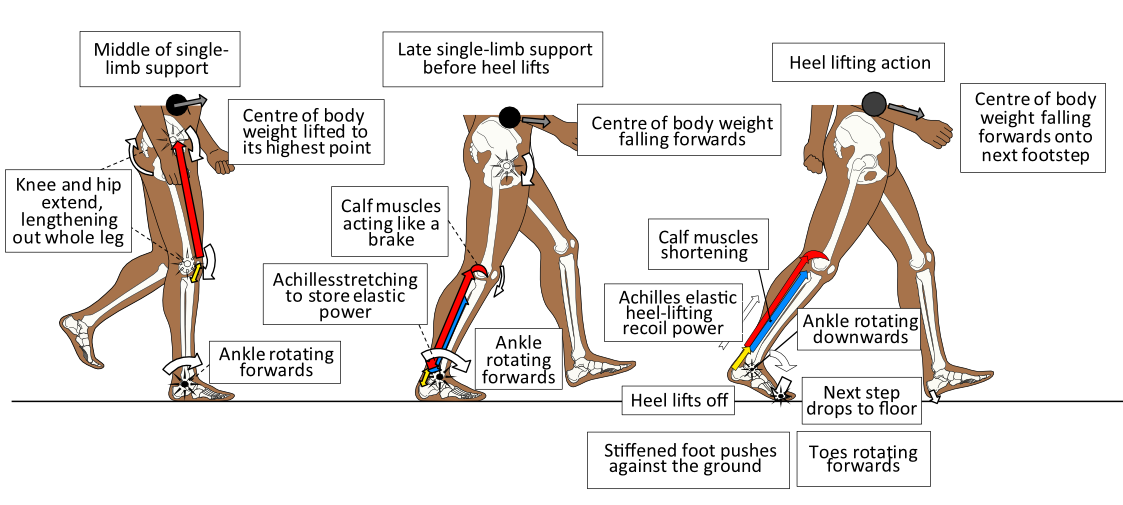
Calf muscles are the big group of muscles found at the back of the leg (or shank). They are associated with the Achilles tendon that sits inferior to them. The Achilles is the thick tendon located at the back of the ankle that attaches to the heel bone (calcaneus). Two powerful calf muscles are attached to the Achilles tendon. This tendon binds firmly to the heel bone and behaves much like a very stiff spring, being stretched when the whole foot is in ground contact. The Achilles is the largest human tendon by cross-sectional area, which tells you that it is very important. Once loaded with elastic stretch energy, it can recoil to lift the heel off the ground as body weight moves towards the forefoot. This occurs just before we make contact with the next footstep, as shown in figure 2.
Figure 2. The calf muscles via the Achilles, are used to control ankle motion while one foot/leg is in ground contact. Release of the stored elastic-stretch energy within the Achilles is used to power forward towards the next step.
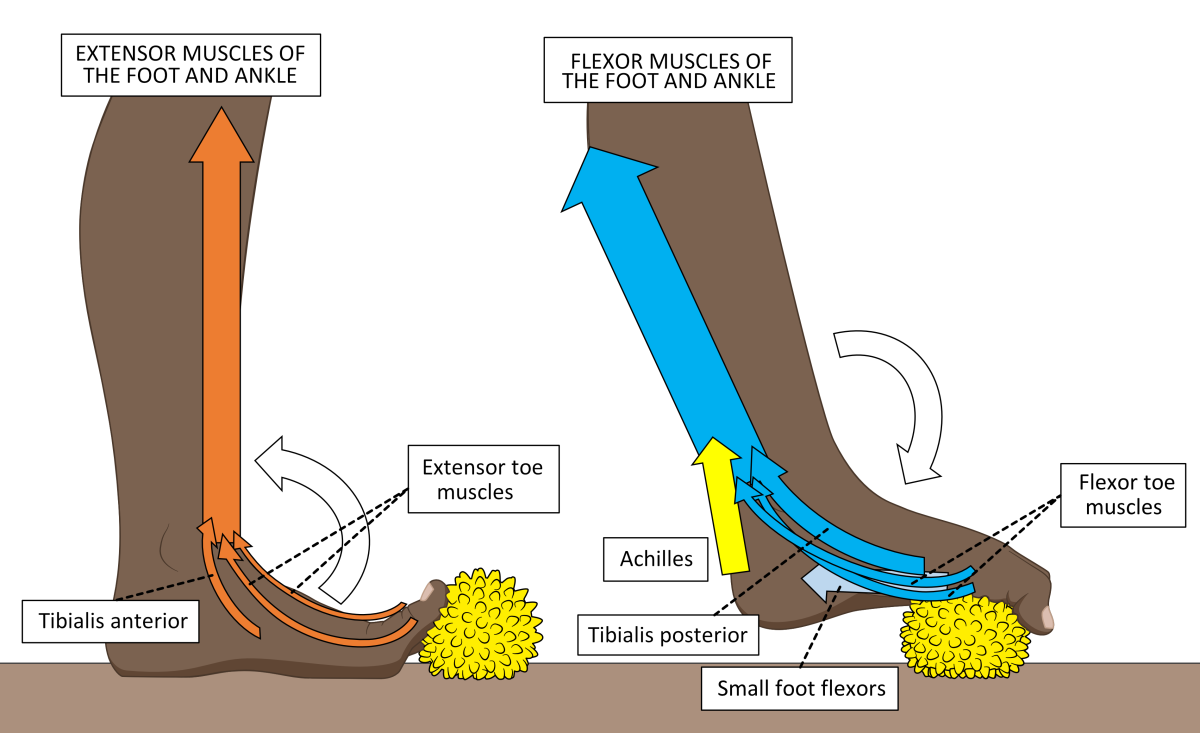
The muscles of the calf that do not attach to the Achilles pass on either the inside or the outside of the ankle, to attach to structures within the foot. Leg muscles include those that pull the toes and foot upwards towards the leg (extensor muscles) or downwards towards the ground (flexor muscles). The extensor muscles are situated on the front and flexor muscles all lie on the back of the shin (tibia) bone. Figure 3 shows how they are worked when using the Healthy Step Foot Exercise Ball.
Figure 3. The Healthy Step Foot Exercise Ball can be used to strengthen both extensor muscles (left) and flexor muscles (right).
During weightbearing activity, these muscles influence how flexible or stiff the foot and ankle behave at any particular moment. Movement around the foot and ankle must be stable enough to stop us from falling over, but sufficiently mobile to allow us to move from step to step over changing terrain. Tibialis posterior is a flexor muscle that plays a very important part in the ability to adjust foot and ankle flexibility and stability.
A rough guide to effective foot function
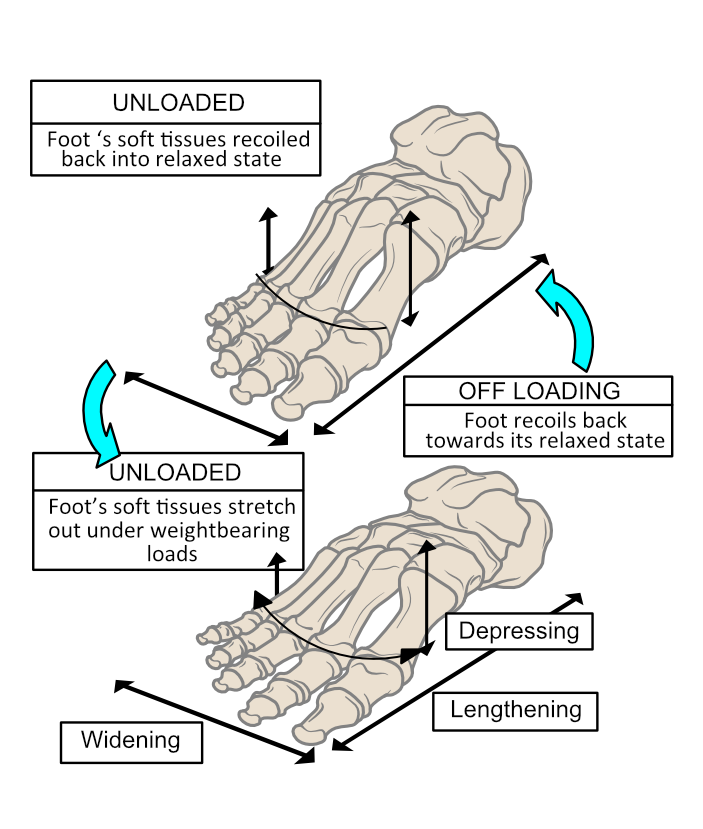
Usually, the heel makes initial contact. Once the forefoot also contacts the ground, the foot’s arched profile lowers rapidly. With all the body weight loaded onto one foot as the opposite leg and foot start to swing forward, the arch is permitted to flatten to allow it to act as a shock absorber. Flattening creates tensions across the soft tissues under the foot bones and also increases the sole’s surface area in contact with the ground. The effect of increasing the contact surface area is to lower the peak pressures generated on the foot’s sole. Pressure is force over area. With more area in contact, forces spread out and peak pressures on tissues under the foot can be better kept within a safe range. Thus, dynamic spring-loaded foot-flattening helps avoid damaging the skin and deep tissues beneath it. As body weight forces unload at the end of the weightbearing phase, the foot can spring back into shape as shown in figure 4.
Figure 4. The foot deforms under body weight, stretching out the soft tissues that hold the foot together. On removing loading forces, the foot can start to spring back into shape with the assistance of important muscles like tibialis posterior.
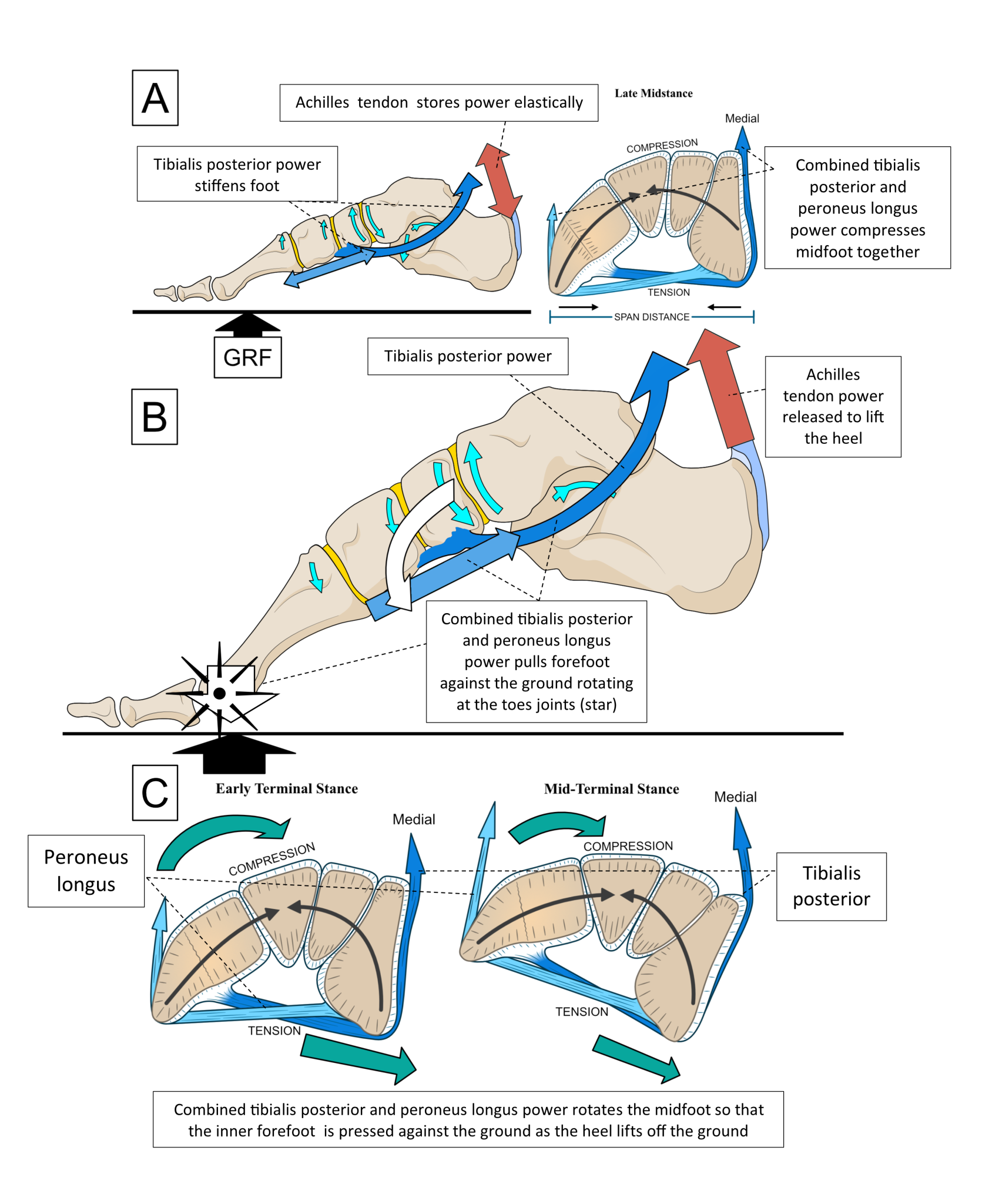
The power to lift the heel off the ground towards the end of any step arises from the stretched Achilles tendon. The Achilles is stretched as the ankle rotates forward with the body passing above and over the single supporting foot. The Achilles tendon should be so full of elastic power towards the end of a footstep, that it wants to pull the heel away from the ground. This becomes easier as body weight moves off the heel towards the forefoot. However, to achieve an efficient heel lift, the foot needs to be semi-stiffened. A stiffer foot means that the forefoot can more easily push against the ground as the heel lifts off, without buckling the foot in the middle.
The foot is supplied with stiffening abilities via the foot-flattening action that causes ligaments and tendons to stretch as well as by activating muscles under it. With a stiffer foot, Achilles tendon elastic recoil power can lift the heel and force the ankle to rotate downwards and forward, pivoting the foot at the big (1st), 2nd, and 3rd toe joints as shown in figure 5.
Figure 5. After the leg has functionally lengthened through hip and knee extension by the middle of single-limb support, the foot increasingly stiffens. Ankle rotation is slowed by calf muscle power as body weight (black spot) falls forward. This action stretches and tensions the Achilles elastically. Once body weight has moved over the forefoot the heel ‘pops up’ off the ground under the recoil power of the Achilles, rotating the foot at the toe joints.
Thus, it is the muscles within the calf and under the foot that control the rate of foot flattening and stiffening during each step. Adaptability in stiffness is necessary because different surfaces under the foot require different degrees of foot flexibility/stiffness. A permanently solid or floppy foot could not provide such necessary variability. Appropriate foot flattening controls peak foot pressures and provides stretching tensions on ligaments and tendons, allowing the foot to act as both a shock absorber and a recoiling spring. Elastic power released under the foot at heel lift ‘recoils’ the foot back into shape after heel lift. Controlling stiffness across the arch appropriately avoids ligament, tendon, and joint damage that could result if the foot squashes down too much or insufficiently.
That’s basically how a foot works!
What does tibialis posterior do?
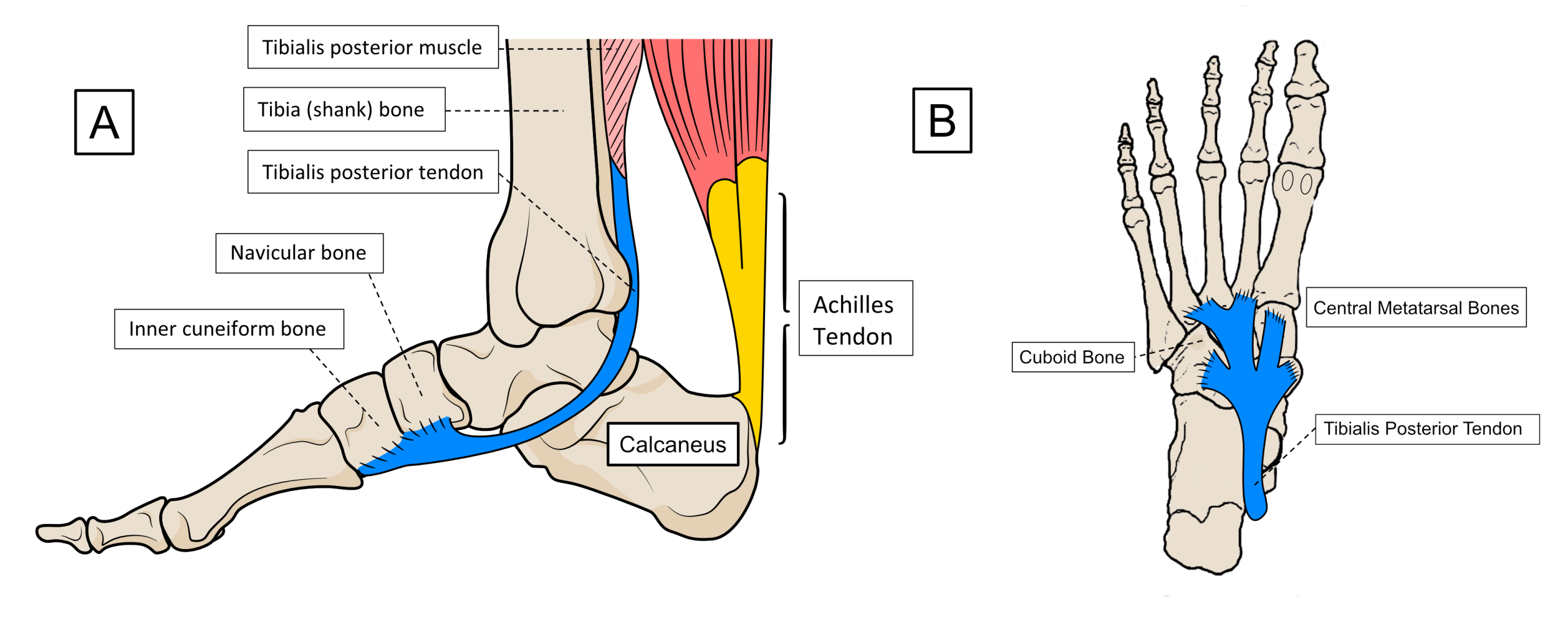
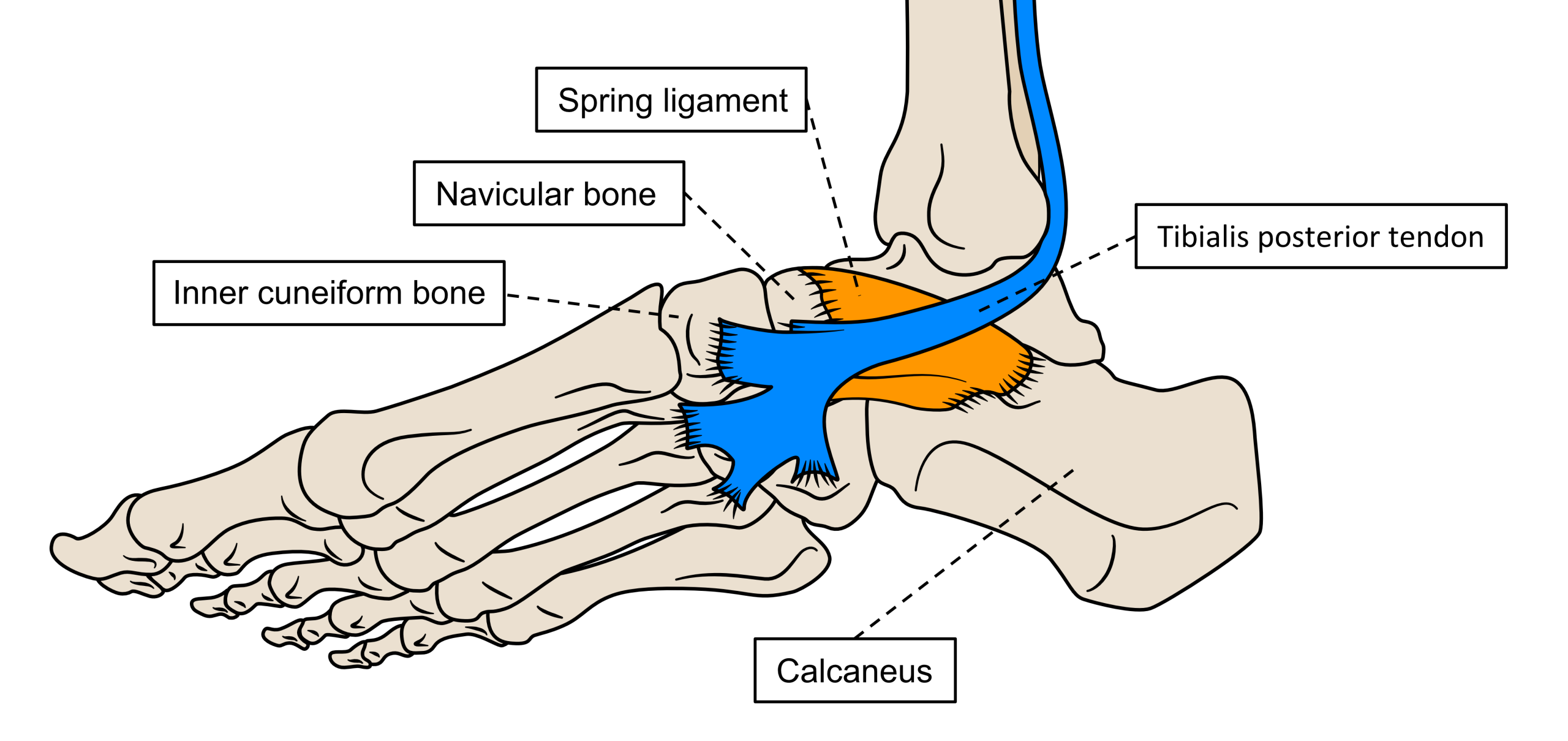
Tibialis posterior is the most important muscle for providing control over the foot’s shape and stiffness changes that must occur when the foot is bearing body weight. It achieves this by running its tendon around the inner ankle bones and attaching it to the inside edge of the foot. It also runs more tendon slips under the foot from the inside towards the outside area, attaching to the underside of most of the bones across the middle of the foot as shown in figure 6.
Figure 6. The inner view of the tibialis posterior tendon (A) and the view under the foot (B).
As tibialis posterior contracts, it compresses its tendon against the inside of the ankle bones and powerfully pulls the foot bones together. To perform its important foot-stiffening role, tibialis posterior works with another muscle found on the outside of the calf.
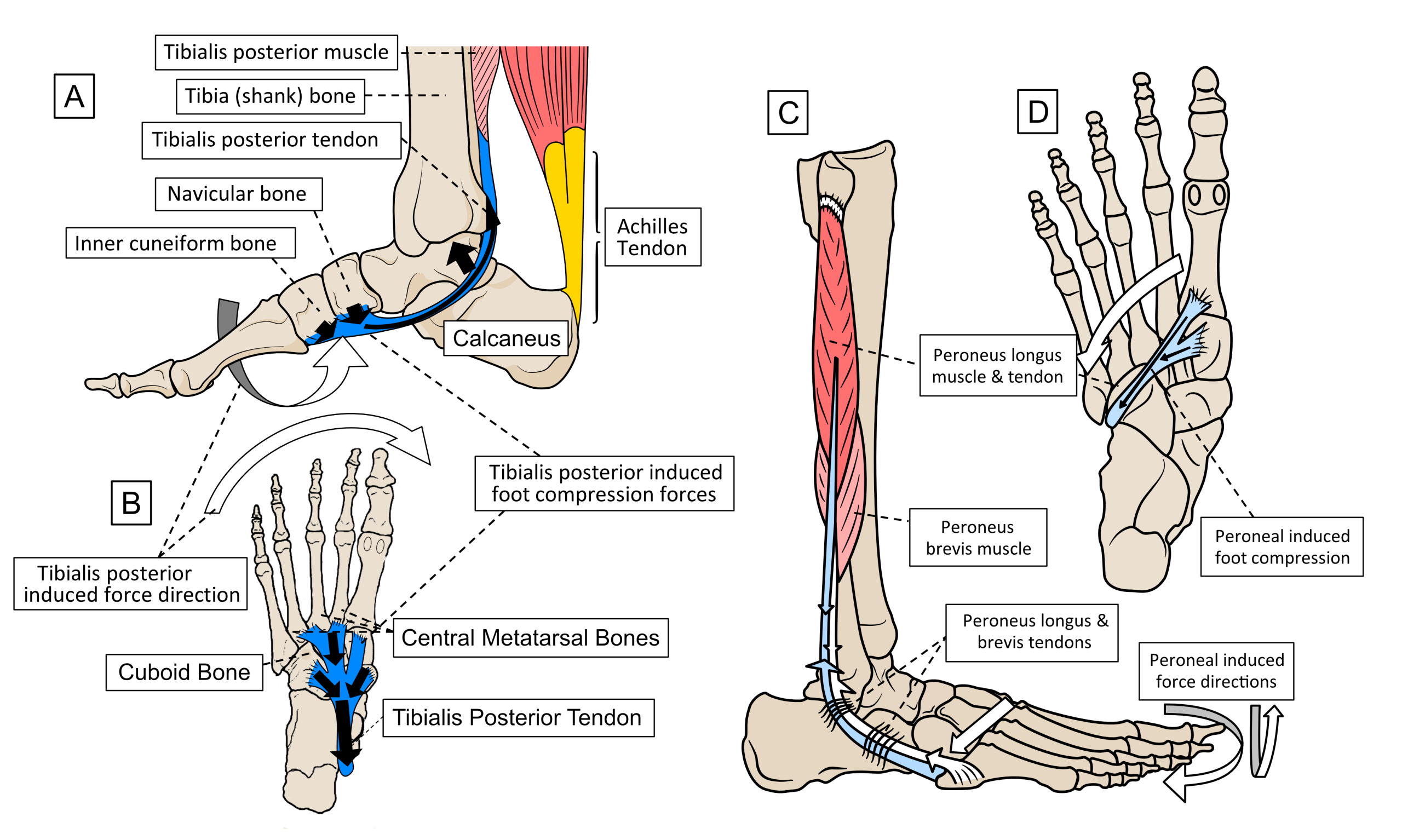
This muscle is called peroneus longus. Peroneus longus runs around the outside of the ankle to pass to the underside of two of the inside foot bones. Together with tibialis posterior, they form a stirrup-like support under the middle of the foot. Tibialis posterior resists any forces that are pulling the foot externally and/or are rotating it inwards at the ankle, while peroneus longus resists motions that pull the foot internally or rotate it outwards. When these muscles work together (and they should always do so) they compress the inside of the foot and ankle bones towards the outside and the outside bones towards the inside ones. This stabilises the foot and ankle like an adaptable brace. Figure 7 shows the position of these two important muscles and the primary forces they generate. Note that peroneus longus has assistance from a smaller muscle called peroneus brevis, to help pull the foot externally outwards.
Figure 7. The location of tibialis posterior’s tendon on the inside of the ankle (A) and under the inside and middle of the foot (B) is shown. The forces created are indicated by the arrows. Peroneus longus’ tendon sits on the outside of the ankle (C), passing under the outside of the foot and running towards the bones on the inside of the arch (D).
Working together, both muscles resist arch lowering against the effects of body weight by setting up forces pulling in opposite directions that compress the foot together and induce arch elastic recoil, once the heel is off the ground.
Tibialis posterior tends to stiffen the foot while peroneus longus will moderate tibialis posterior’s stiffening capacity to stop the foot from becoming too rigid. When these muscles relax the foot becomes more flexible. If tibialis posterior works harder than peroneus longus, the foot tends to stiffen excessively, especially along the inside edge. However, if peroneus longus works harder than tibialis posterior, the foot becomes more flexible along its inside edge.
Together, the power derived from these two muscles helps pull the forefoot firmly downwards against the ground and tips the foot towards the big toe and 2nd toe joints at heel lift. These two toe joints are the most mechanically efficient joints used to drive forward from onto the next step. More detail is shown in figure 8.
Figure 8. Before the heel lifts (A), tibialis posterior and peroneus longus muscles’ powerfully compresses the foot together, making it more elastic and less flexible as it flattens down. As the heel springs up (B), the midfoot moves downwards and rotates via tibialis posterior power (C). More pressure is now exerted on the inner forefoot area around the big toe joint and its neighbours. These toe joints (see the star in B) now allow the rest of the foot to rotate upwards, over, and around them until the toes leave the ground too.
Tibialis posterior and the spring ligament in supporting the arch
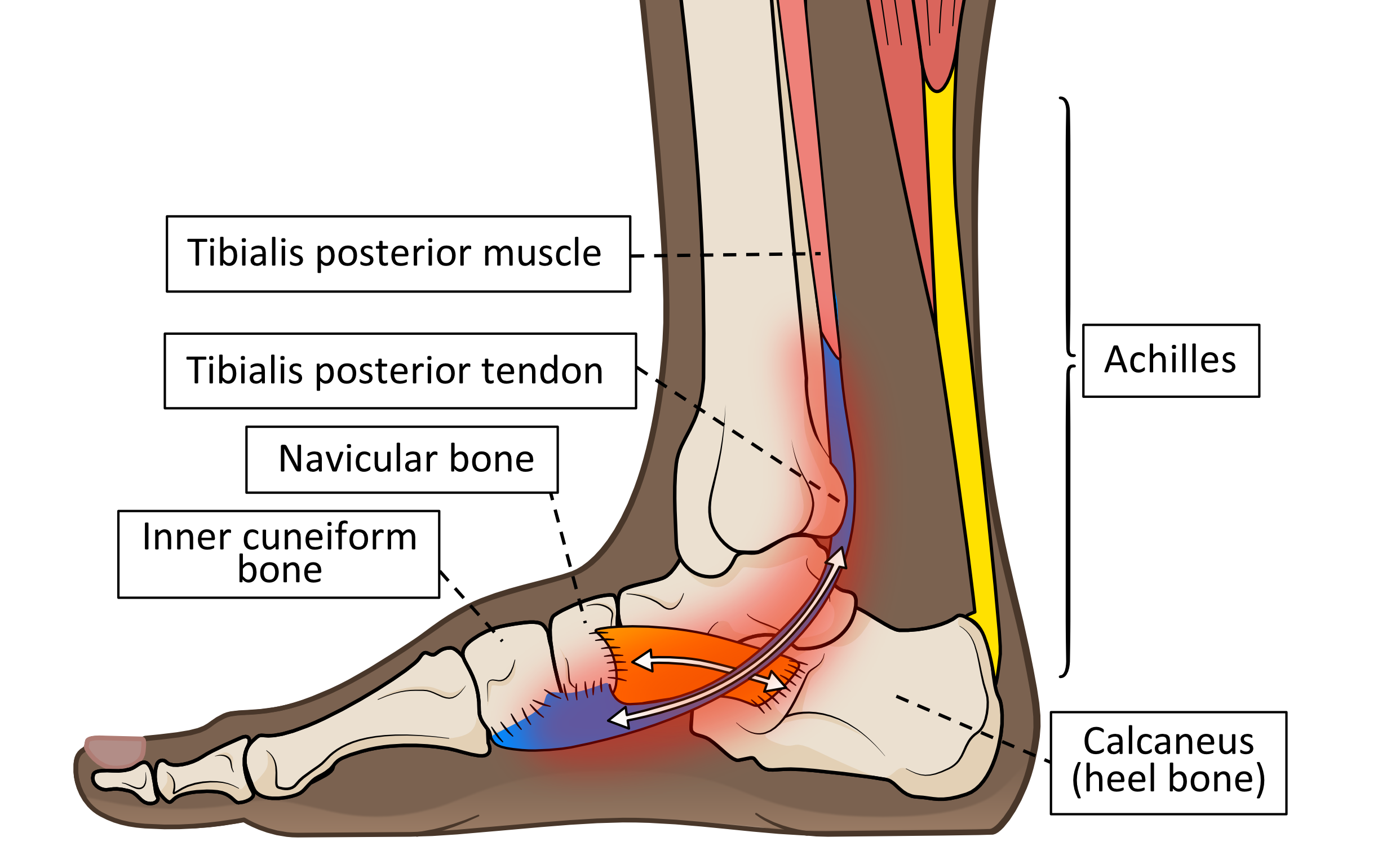
Tibialis posterior attaches its tendon to an important ligament that lies under the inside edge of the foot which assists in reinforcing ankle and arch stability. This ligament is commonly known as the spring ligament as shown in figure 9.
Figure 9. The spring ligament is a complex of connective tissue fibres that support the important joint lying between the ankle, the navicular bone, and the calcaneus (heel) bone. Tibialis posterior’s tendon attaches to the spring ligament before it passes to support the bones in front.
The spring ligament and tibialis posterior are important in maintaining the highest parts of the natural vault-like profile under the foot. This concave contouring is commonly called ‘the arch’ of the foot, although it is more shaped like a 3-dimensional dome or vault. Humans have an arch for several reasons that enhance the foot’s mechanical properties during each footstep. This includes aiding the foot to provide spring-like properties. The arch should be able to squash down and then spring back into shape.
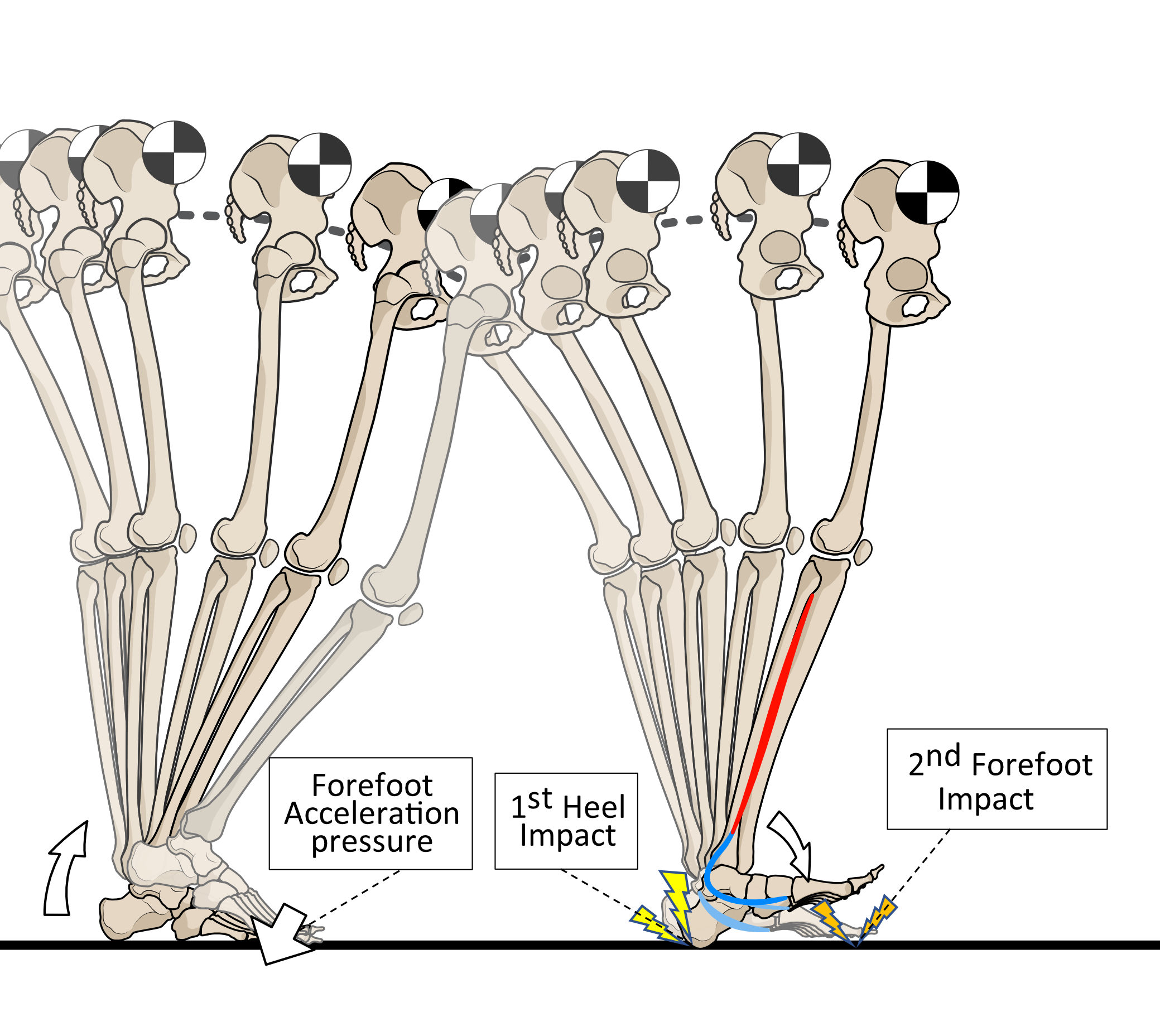
Having a vault profile in the middle of the foot creates distinct heel and forefoot areas. This allows the foot to hit the ground twice. First via the heel impact to then be followed a little later by a separate forefoot collision. Such an approach divides the collision forces of ground contact into two smaller-force events rather than having a single bigger impact, as shown in figure 10.
Figure 10. After forces are applied to the forefoot of one foot via heel lifting power, the opposite foot makes ground contact. First hitting the ground via the heel and then the forefoot divides impact into two lower collision forces. For this process to work properly, tibialis posterior activity is required.
Tibialis posterior acting with the spring ligament provides the bulk of the active power to control the stresses being applied across the foot’s arch as the forefoot hits the ground. Together, tibialis posterior’s tendon and the spring ligament absorb impact forces and continue to stretch out as full body weight is loaded onto the foot. Without tibialis posterior power being applied to the foot appropriately via the spring ligament, it is extremely difficult for the foot to offer a stable shock-absorbing base for the body to rotate forward over and then to accelerate forward from.
What is tibialis posterior dysfunction (TPD)?
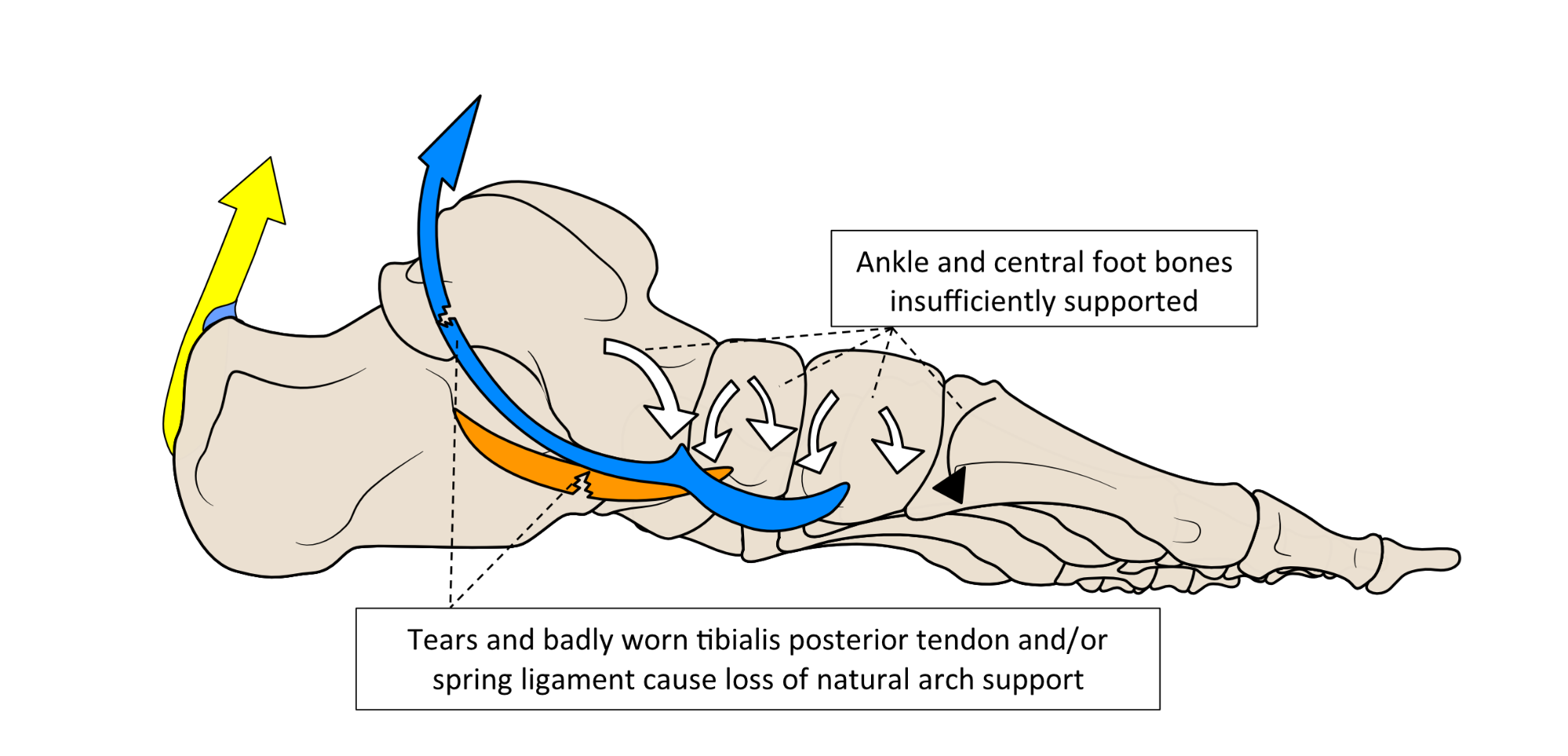
TPD (or PTTD) is a condition where tibialis posterior is not providing the level of power to stiffen the foot and stabilise the inside of the ankle sufficiently. This could be a result of weakening of the muscle itself, its tendon being damaged, or because the spring ligament has torn.
If the spring ligament is torn, the full power of tibialis posterior cannot be applied effectively. As a result of the ligament not controlling local bone motion, more stress is directly placed upon tibialis posterior’s tendon. Failure of the spring ligament’s ability to hold the bones just in front of the inside of the ankle will mean loss of the ability of tibialis posterior to stiffen this area sufficiently to prevent the foot’s vault profile from flattening excessively.
Thus, both damage to any part of tibialis posterior or the spring ligament allows the ankle and arch to roll inwards and the foot to flatten more than it should. This will cause abnormal straining of other soft tissues and joints across the foot. Thus, spring ligament injuries result in TPD and TPD causes spring ligament injuries.
What happens as a result of TPD?
All the benefits derived from controlled foot-flattening and stiffening, such as the shock absorbing and spring-recoil abilities are lost with TPD. The foot starts to flatten too quickly and excessively as the forefoot makes its ground contact. This situation worsens as heel lift is approached, as shown in figure 11.
Figure 11. Without a strong tibialis posterior tendon and spring ligament, the foot flattens inwards, especially as heel lifting forces rise.
Because the tendon of tibialis posterior also helps stabilise the medial side of the ankle, loss of its power causes the ankle and heel to roll inwards as the foot flattens excessively. TPD causes loss of the lateral (outside) to medial (inside) stirrup-like compression stability across the foot and ankle. The foot can now collapse in the middle when weight is placed upon it, an event that is most dramatic as the heel attempts to lift.
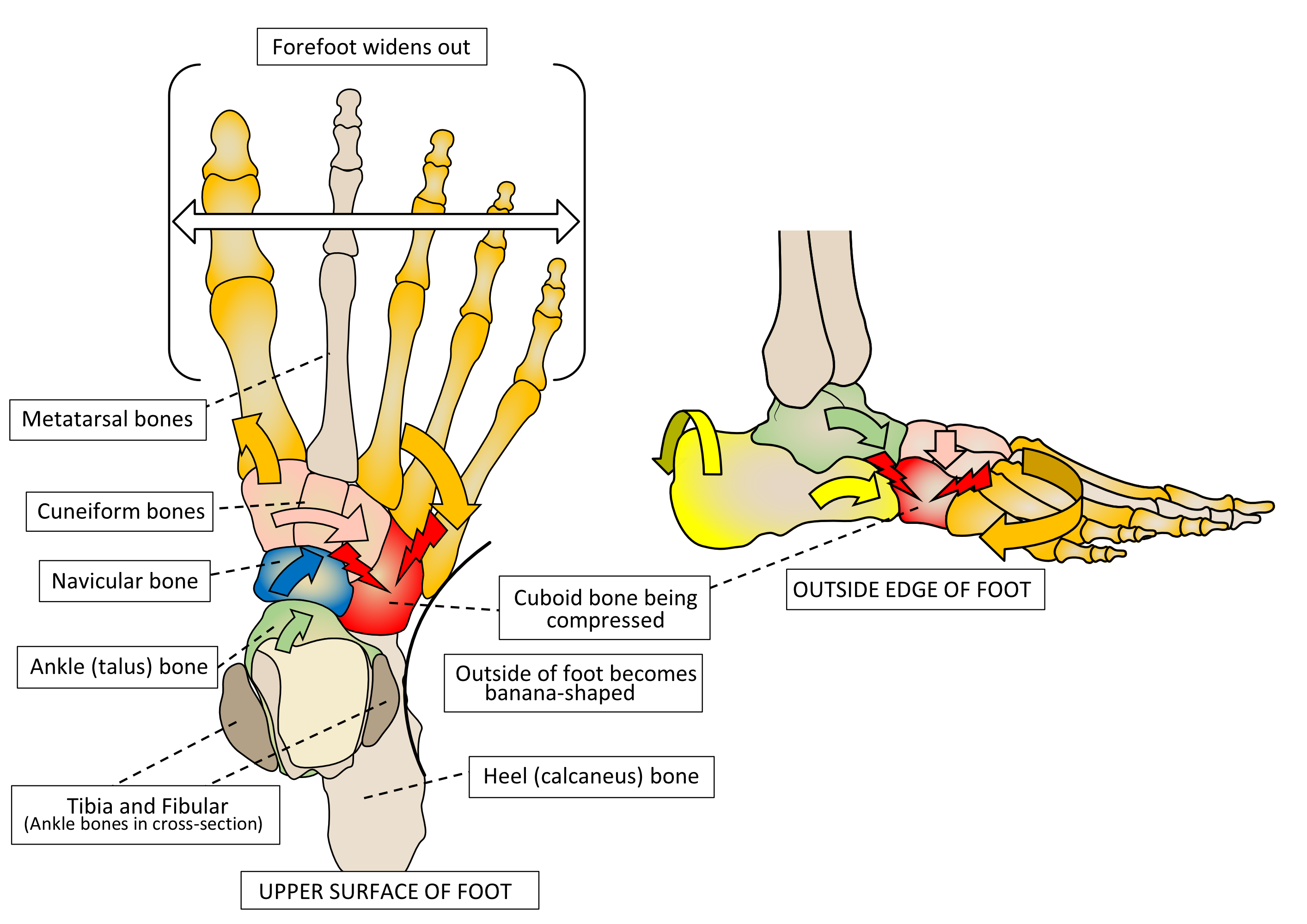
In TPD, peroneus longus continues to pull the midfoot and forefoot outwards, but this action is no longer resisted. Thus, the rearfoot starts to bow inwards, while the midfoot and forefoot start to drift outwards, giving the outside edge of the foot a concave or banana-shaped appearance, as shown in figure 12.
Figure 12. Some suffers of TPD can cause ‘bowing’ that causes the bones on the outside of the foot to compress together. This can cause discomfort here.
These events all put a lot of extra stress on the soft tissues that resist foot flattening and inward ankle and rearfoot motions. This includes the tibialis posterior tendon and the spring ligament themselves. Pain on the inside of the ankle during and after exercise is usually the first and primary symptom of TPD, because the tibialis posterior tendon lies as shown in hazy-red area of figure 13.
Figure 13. Pain usually starts somewhere within the hazy-red area that matches the tendon position underneath.
Because the arch flattens and becomes too mobile, other ligaments and muscles that help support the ‘arch’ profile can become over-strained too. As a result, aches under the foot are common symptoms of TPD. Usually, once ‘arch’ pains start, the TPD sufferer becomes aware that their foot profile has started to change, as shown in figure 14.
Figure 14. As the foot profile alters, tibialis posterior’s tendon and the spring ligament come under increasing strain that provoke pain and weakness.
As a result of TPD, the forefoot becomes too flexible. As the heel lifts, the foot starts to buckle in the middle and tilts inwards rather than rising onto the forefoot.
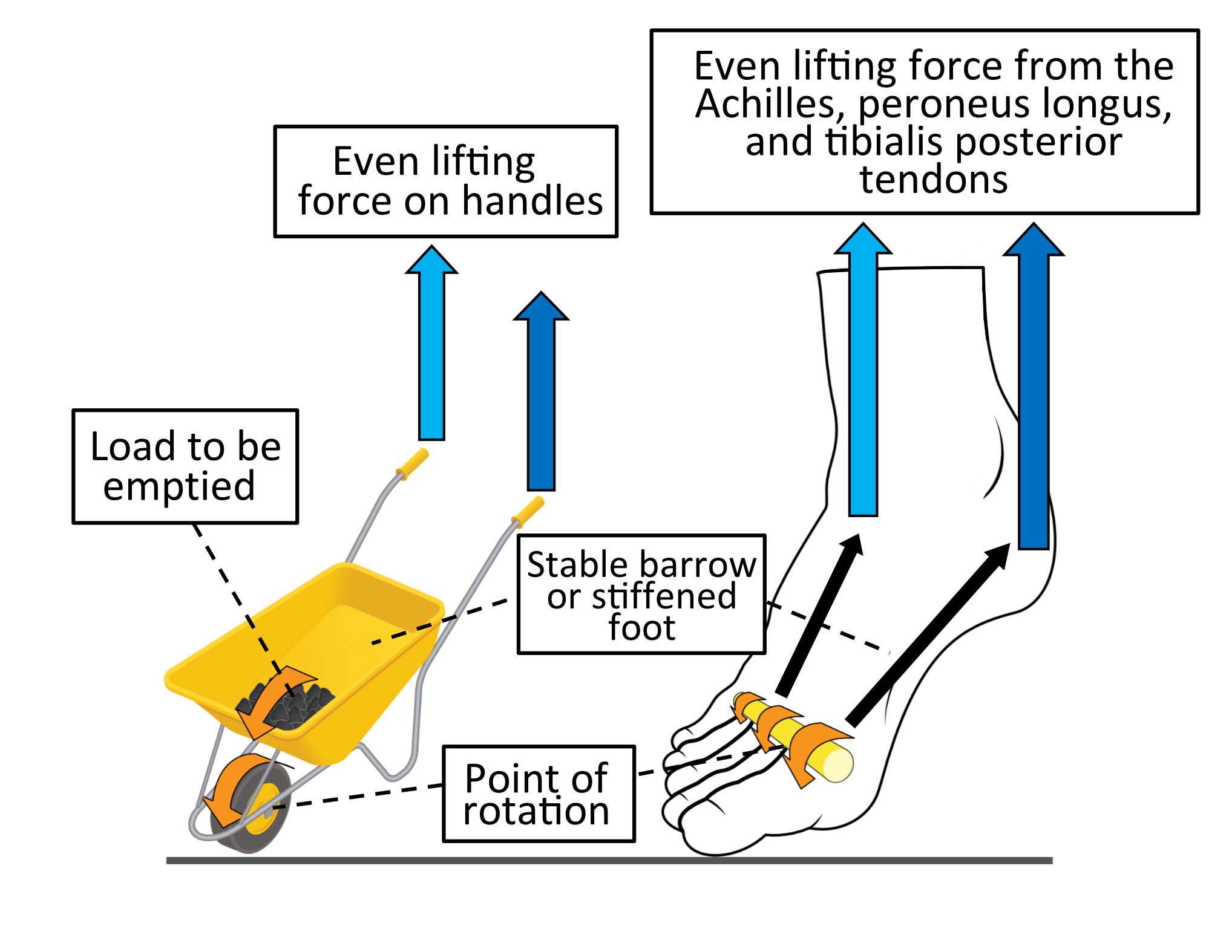
A simple analogy is to consider how a wheelbarrow is emptied. Normally the load is tipped out by lifting both handles evenly to rotate the wheelbarrow at the wheel, allowing the load to empty in a forward direction. The Achilles tendon power with tibialis posterior and peroneus longus working together equates to lifting both handles with equal force as shown in figure 15.
Figure 15. Lifting handles with equal force on a wheelbarrow tips the contents out straight ahead. Peroneus longus force is indicated by the light blue arrow matching in size those from tibialis posterior (dark blue arrow).
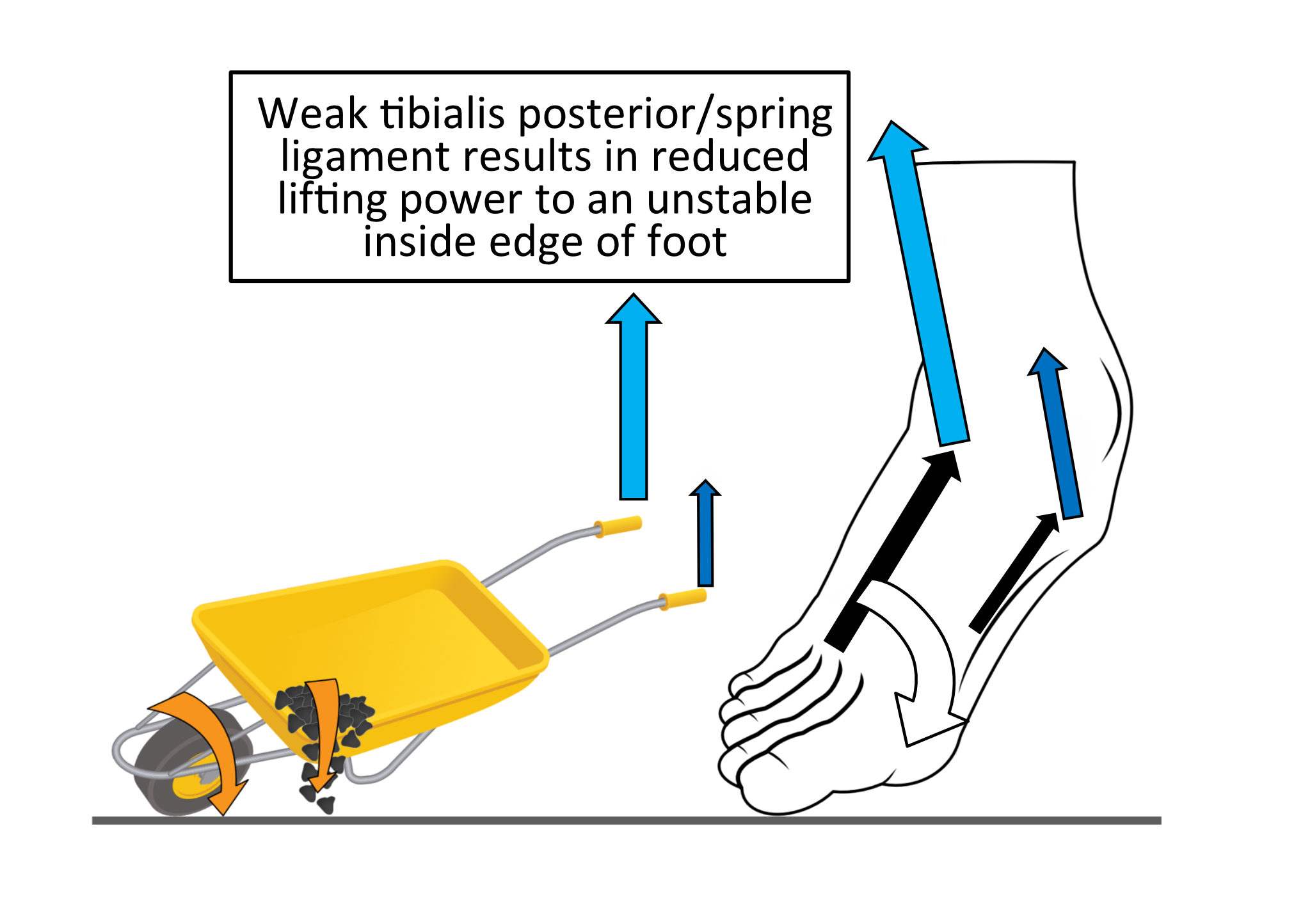
Lifting the load using most force on just one handle will cause the wheelbarrow to fall towards the opposite side. This equates to losing tibialis posterior power on the inside of the ankle. Lifting the heel with just Achilles and peroneus longus power, causes the foot to roll inwards as the heel lifts as shown in figure 16.
Figure 16. Lifting handles with asymmetrical force on a wheelbarrow tips the contents towards one side. This is a similar effect to TPD producing weaker forces (smaller dark blue arrow) with peroneus longus forces (light blue arrow) remaining normal.
Overall, TPD creates a less adaptable flatter foot that is too flexible to act as either a shock absorber or an acceleration spring. This means that stresses across the foot are poorly managed. As a result, sufferers of TPD tend to feel that their affected foot feels weak and unstable.
In time, TPD can become a significant disability that is very difficult to fully resolve. Catching it early is essential to a good outcome.
Why does tibialis posterior dysfunction happen
TPD is commonly a result of degeneration of the tibialis posterior tendon, especially within the areas where the tendon is put under compression around the medial side (inside) of the ankle and foot. These areas are mechanical weak points because where tendons wrap around bone, they have to be packed with softer fibrocartilage to resist compression. Although much better at resisting compression, these areas are not as good as normal tendon in resisting tension. As a result, these areas are more prone to wear away.
The superior inner part of the spring ligament is also supplied with fibrocartilage because it receives a lot of compressive stress from the bones above it being forced downwards an inwards during weightbearing. This makes the inner area of the spring ligament more vulnerable to degeneration than other parts.
Damaged ligaments within the foot vault cause increased strain on tibialis posterior, in particular the spring ligament although other ligaments in the area can be at fault. Ligament damage can be caused by an acute high-stress event on the foot (consider previous ankle sprains) or from age-related degenerative changes.
What is clear from the science is that problems with tibialis posterior increases stress on the spring ligament, and issues with the spring ligament increases stress on tibialis posterior and its tendon. Thus, once problems start in one, a dangerous cycle of raising stresses on supporting tissue and increasing loss of ‘arch’ control is set up.
As animals age, the elastic behaviour of their fibrous tissue such as tendons and ligaments become stiffer, more brittle, and less elastic. Therefore, the tibialis posterior tendon and the spring ligament become naturally weaker with age. Thus, most cases of TPD are in part age related.
Diabetes is a particular problem because it causes premature soft tissue ageing. Also being significantly overweight and menopausal are poor combinations, as high body weight causes increased stresses on the feet while the loss of protective hormones causes increasingly brittle and inelastic tendons.
However, problems can also be induced by issues such as unstable footwear selection that force muscles to work abnormally. Having weak foot muscles is also a risk factor. Sudden increased activity can initiate or reveal tendon/ligament damage or weakness in older individuals, so often symptoms start during or after an increase in exercise levels.
Certain rheumatological diseases such as rheumatoid arthritis, can also cause TPD, and this can affect younger people. Rheumatic diseases cause the immune system to attack joints made of cartilage within the body. Therefore, areas of tendon or ligament made with a lot of fibrocartilage inside them are vulnerable to attack too. Both tibialis posterior’s tendon and the spring ligament have areas within them that possess high fibrocartilage content, so that the immune system may attack and damage these areas, weakening them.
Usually, TPD is very rare under 30 years-of-age because tendons are kept very healthy in the young (unless there is a disease). If problems arise in younger individuals, it is usually a result of inflammation in a protective lubricant-filled sheath that lies over the tendon to stop friction as it moves within the tissues. This is known as tibialis posterior tenosynovitis. It usually results from increasing activity such as long-distance running, with insufficient strength among the foot and ankle muscles (particularly tibialis posterior itself). Its far less serious and easier to treat, unless it is left unresolved and becomes chronic.
Treating TPD
TPD causes pain on the inside of the ankle that radiates into the medial side of the foot, with concurrent excessive flexibility across the ‘arch’ that permits increased flattening as shown in figure 17.
Figure 17. The flattened foot and pain location that arises from TPD.
Just as important as the local pain is the concurrent loss of tibialis posterior’s power. This reduces the ability of the foot to shock absorb during loading under body weight. The foot also loses the ability to ‘stiffen-up’ to make a firmer forefoot platform to accelerate off the ground. Overtime, TPD weakness increases flat footedness. TPD always requires treatment urgently.
IMPORTANT: BE AWARE!
Sometimes TPD develops without much or any pain. Instead, the suffer notes a change in foot profile when standing and walking, often with a feeling of weakness/instability.
Always find out the reason why your foot is changing shape.
Lowering or raising of the foot arch profile is often an indication of something serious happening. See a foot health professional for advice as quickly as you can, even if there is no pain or discomfort.
Key Solutions for TPD:
- To treat TPD problems, the arch of the foot must be supported.
- If possible, the strength of tibialis posterior should be improved.
- The surrounding supportive muscles must also be strengthened.
- The correct footwear styles should be used to help stabilise the foot.
The ability to resolve, rather than just manage TPD is dependent on how quickly it is treated. The longer it persists, the more permanent the damage to the tendon or spring ligament. Tendons are very difficult to heal and a damaged tendon loses its ability to stretch and recoil like a spring.
Treatment of early (acute) stages:
If TPD pain has been occurring for less than 6 weeks and the foot profile still appears normal on standing, there is a good chance that with the correct treatment the problem can be solved. Take action now!
- Start using supportive footwear. Ideally, they should have fastenings, (laces being the best option) and a small raise on the heel compared to the forefoot, rather than being completely flat.
- The shoe should only flex across the toe joint area. The shoe should be difficult to flex or twist anywhere but at this forefoot flexion point.
- Most trainers are usually ideal, as are many comfort-styled shoes.
- Start foot rehabilitation exercises:
- Consider an arch supporting insoles such as those from the X-Line™ range of insoles produced by Healthy Step™. In the early stages, the TPD50® is a great choice.
Once pain has resolved for at least 4 weeks, you may find than an X-Line RIF® insole may offer all the support you require in the longer term. Just keep X-Line RIF® in all the shoes you walk in regularly, and you should stay out of trouble in the longer term.
To help to protect your feet long term, regularly use the exercises recommended by Healthy Step above.
Treatment of late (chronic) stages:
If TPD has been occurring over 6 weeks, chances are that some significant tendon damage has already occurred. We would advise that you seek some professional foot rehabilitation advice.
You might have noticed that the foot profile looks flatter on the affected foot than does the other when standing. However, if the foot returns to its usual non-weightbearing appearance when offloaded, there is still a chance to fully resolve the problem.
- An X-line TPD® is recommended, as this offers the most support to the arch of the foot.
- Select shoes that are firm and supportive with lots of lace holes. Lace up ankle boots can be particularly helpful as long as they only flex across the toe joints.
If the foot profile is flatter than the unaffected side and remains flatter-looking when the affected foot is lifted from the ground, the chances are that the tendon has been damaged permanently.
If this is the case, you are likely to require insoles forever for walking. The Healthy Step vectorthotic® range is a good choice, but you will need provision or prescription through a health care profession.
Treatment of long standing (chronic) stages
Long standing TPD causes the foot to permanently become flattened without elastic recoil. The foot will be fixed into this flattened deformity, both non-weightbearing and weightbearing.
This makes walking far more difficult and the use of supportive shoes and insoles will be necessary forever more.
Because such feet are challenging to make comfortable, these feet require something bespoke (custom made) or custom adjusted to fit the foot. These cases will require clinical support from a foot health professional with experience in dealing with this disability. In some cases, surgery can help but even then, the foot will never be as functional as it once was.
This is why early treatment and resolution of TPD is essential.
Tenosynovitis in tibialis posterior tendon
For tenosynovitis reducing activity, using support insoles such as the X-Line TPD50®, and strengthening the foot and ankle muscles usually resolves the problem. In most cases, supportive insole use is temporary, although it can be wise to continue to use less supportive insoles for activity that triggered the problem initially in future.
- Use X-Line TPD50® until the pain fully resolves and for at least 2 weeks after.
- Strengthen your feet with exercises as listed above.
- Use a simple supportive insole such as the Arch Angel® for running or long-distance walking to help prevent strain on the tibialis posterior in future.
If not quickly resolved, tibialis posterior tenosynovitis can lead to tendon damage that risks full TPD developing.
Medial ankle pain should always be investigated even in the young and active, because of the potential for this minor problem to become a serious condition that affects mobility permanently.
Sources of Information
The information provide here was sourced from the two medical textbooks. Both books are extensively referenced from peer review medical and scientific literature, and are published by Academic Press, an imprint of Elsevier.
Clinical Biomechanics in Human Locomotion: Origins and Principles.
Andrew Horwood, with contributions from Nachiappan Chockalingam
ISBN 978-0-323-85212-8
Clinical Biomechanics in Human Locomotion: Gait and Pathomechanical Principles.
Andrew Horwood, with contributions from Nachiappan Chockalingam
ISBN 978-0-443-15860-5
Both textbooks are available directly from the publisher or through other online and academic book retailers. They are written for a medical audience with some prior anatomical knowledge.