Plantar fasciitis: A pain in the heel!
Introduction
Plantar fasciitis is the most common cause of plantar heel pain on the sole of the foot. However, not all plantar heel pain is plantar fasciitis.
Pain first thing in the morning on standing down or rising from sitting at any time of the day, are the classic signs of plantar fasciitis. Initially, walking and moving around will often seem to take the pain away. However, symptoms are often worse after more weightbearing exercises (e.g., walking or running). In time, pain in the heel can also develop towards the end of extended periods of exercise.
Other causes of plantar heel pain tend to present with a different pattern of pain. Alternative heel pain sources include plantar fat pad atrophy, heel bone (calcaneus) stress fractures, and heel neuromas/nerve entrapments. Night pain within the heel at rest is associated with heel bone (calcaneus) tumours or arises from referred symptoms from the sciatic nerve (radiculopathy). These conditions consisting of rest pain can affect any age, including children.
Children with heel pain associated with exercise, often have a condition known as Sever’s which is triggered by excessive stresses on growing heel bone. Plantar fasciitis is a degenerative condition that does not normally affect children.
Where is the plantar fascia and why is it important?
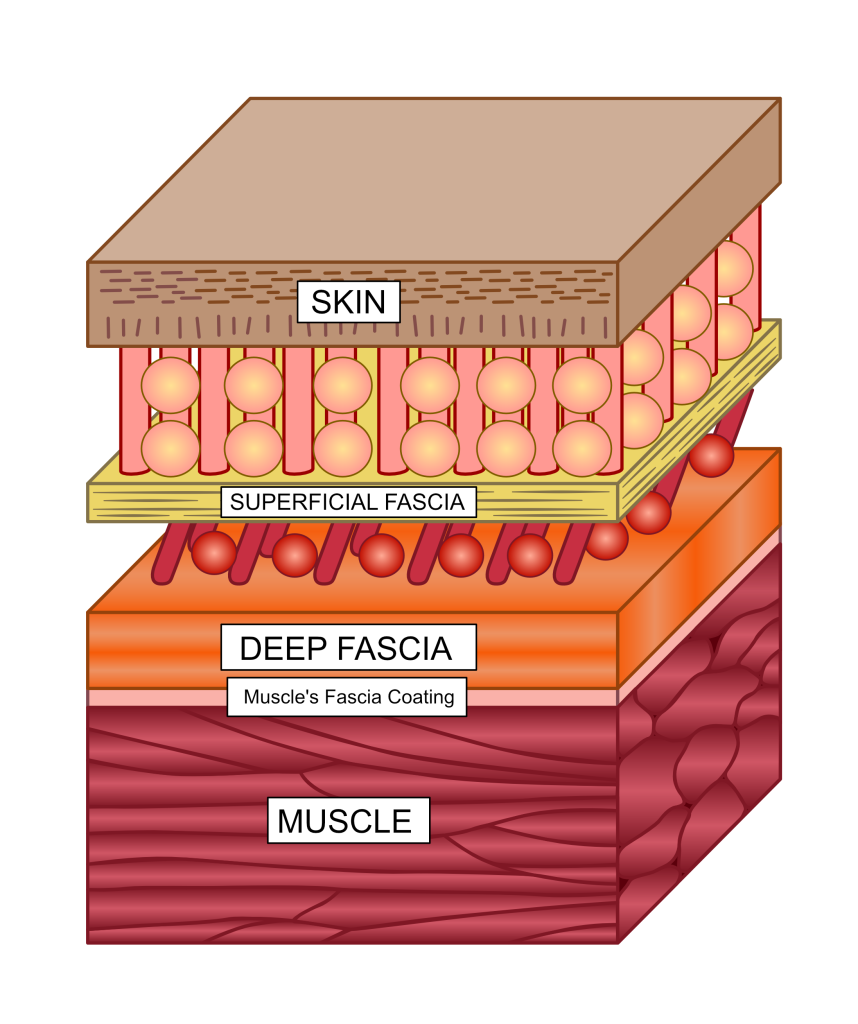
The plantar fascia is a thickened band of connective tissue located under the skin of the sole of the foot. Fascia is a thin tissue made of materials that are also found in other connective tissues, such as tendons and ligaments. Fascia forms tubes and sheets that wrap around and between muscles and other anatomy. It also forms a complete covering of all the anatomy beneath the skin, much like a very thin, tight wetsuit. This is known as deep fascia. There is also another more flexible fascial layer bound under the skin that allows the skin to move over the deep fascia relatively freely. This is the superficial fascia. The loose union between deep and superficial fascia forms a weak point where skin can be removed from an animal most easily, an act known as flaying or skinning. See Fig 1 for where fascia sits under the skin but over the muscles.
Figure 1. Deep fascia, which the plantar fascia is part of, is found lying over muscles but lying deep to the superficial fascia under the skin. The red zone here between the different fascia is the weak point used for skinning.
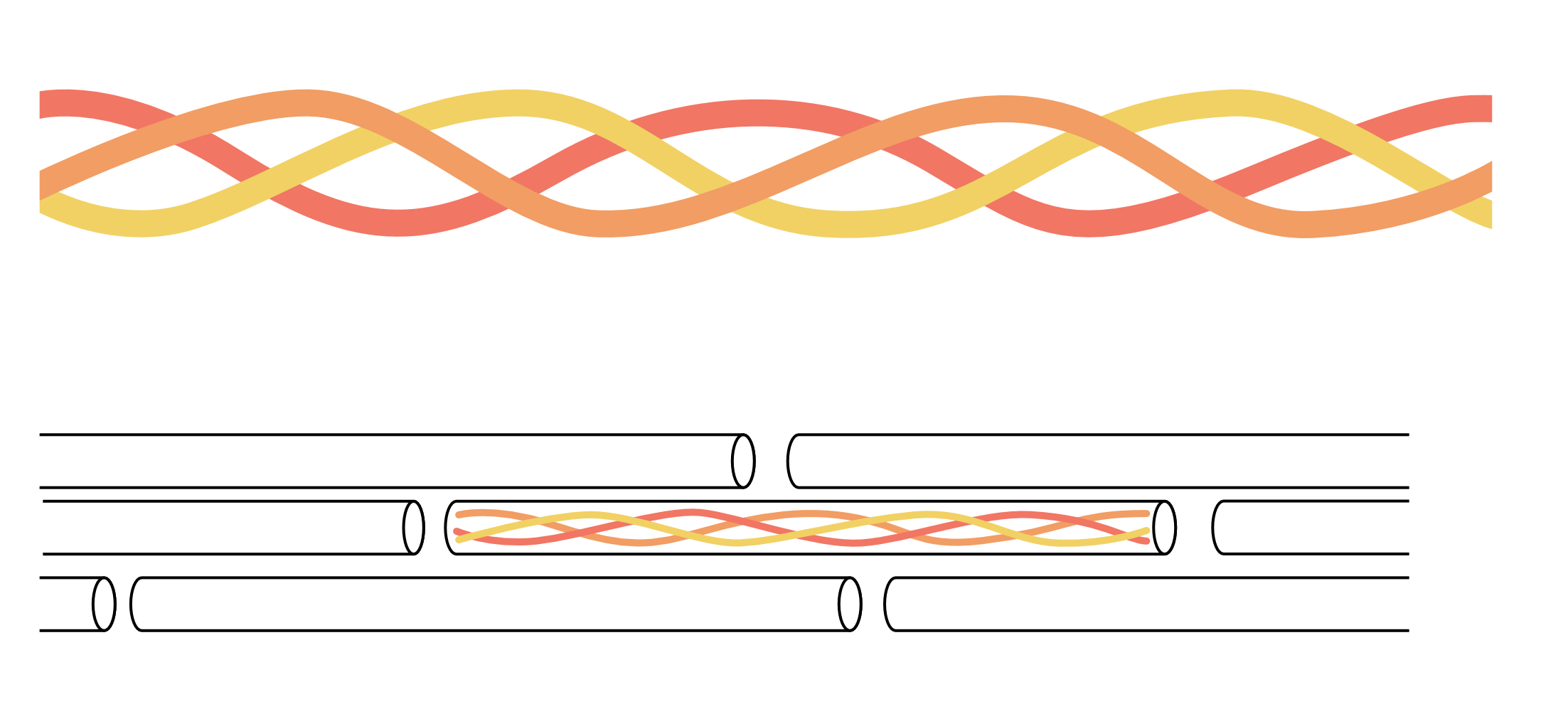
Fascia, tendon, and ligaments all contain lots of collagen. Collagen is a very strong protein that usually forms from a twisted protein chain that then twists together with other collagen into a stiff spring-like microfibre formed by three chains winding around each other. The microfibres then form together to construct larger fibres to create more flexible spring-like properties within the complete connective tissue. See Fig. 2.
Figure 2. Collagen proteins form twisted structures that create three twisted chains bound together to construct a spring-like microfibre (top image). They then organise into a highly structured arrangement of larger groups to form collagen fibres of connective tissues that can stretch a recoil. It is the twists within the basic building blocks of collagen and the fact fibres can move separately from each other, that underpins the spring-like behaviour of tendons, ligaments, and fascia.
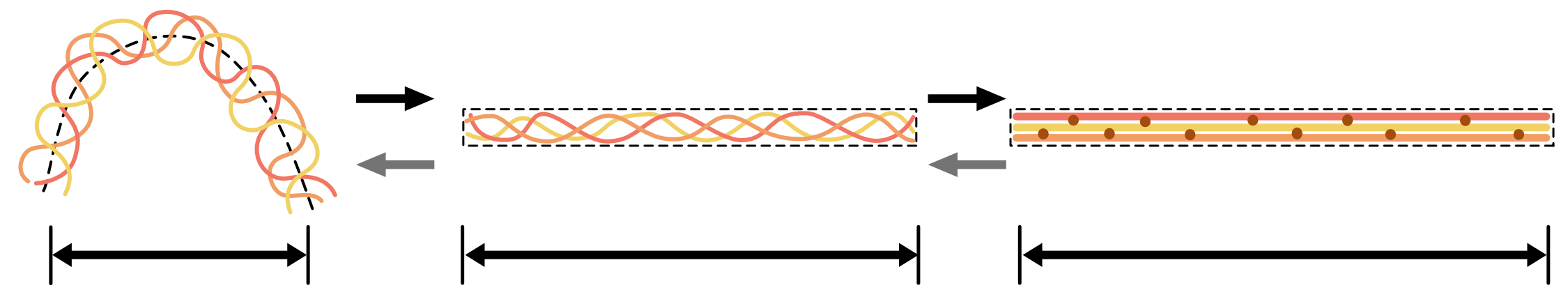
Thus, fascia tightens when tensioned and recoils when stress is released. Just like a steel spring, the more it stretches the stiffer it behaves. In many respects, collagen is the biological steel that provides strength to the body’s tissues and just as steel can be formed into springs by twisting rods made of it, so collagen fibres are usually formed in a twisted spring-like manner, as demonstrated in Fig. 3.
Figure 3. At rest and relaxed, collagen microfibres form crumpled arrangements of springs within the connective tissues. However, once under tension (arrows to right) they quickly become taught and start to act like linear springs, gradually stiffening and storing elastic energy. Once offloaded (arrows to left), they spring back to their resting position. This is as long as they have not been damaged when under tension.
Collagen makes billions of fibres across the body that vary in their orientation. The fibres are bound together among living cells by flexible biological glue, known as extracellular matrix. By packing in more collagen fibres and arranging them in specific directions, some connective tissues become more structured than others. For example, tendons are very densely packed and highly structured, with fibre orientations that give them great strength in just one direction of tension.
Tendons are very special connective tissues that link muscles to bone. Their collagen fibres nearly all run in the same direction to the muscle’s generated force so that tension can be directed to create or resist a specific motion. Ligaments bind bone to bone around one or more joints. Collagen fibres in ligaments are more variably orientated across different areas of them, reflecting the more variable tensional forces that are applied around and across joints to guide, rather than stop motion. This is because most joints are capable of moving in several directions at the same time.
Fascia has the most diverse fibre arrangements. However, in any particular area, fascia’s fibres still dominate in the direction that most tensional forces are applied across it. Most tension forces arise from the muscles contracting and joints moving beneath each area of fascia. Superficial fascia requires the greatest variability in fibre orientation as skin stretches in all directions. Even then, each area of skin tends to experience some force directions more frequently than others. As a result, even superficial fascia orientates fibres primarily to resist the commonest tensions they experience.
Areas of thickened superficial fascia can form after injury causing less stretchy skin, known as scars. Although we cannot see it, scar tissue formation occurs in deep facia after injury too, and its presence changes how freely fascia can stretch and move over a larger surrounding area. In time, scar tissue should become better organised to act mechanically more like the original and surrounding fascia did. This explains why scars on the skin usually become less noticeable as the years go by. However, that does not always happen.
Fascia’s role
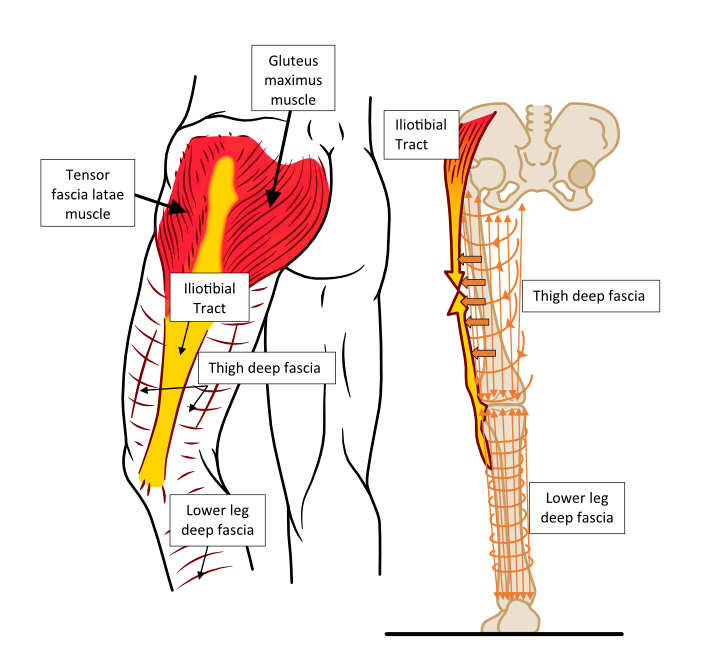
The lower limb’s deep fascia fibres most commonly orientate in an up-down direction (from head to ankle) because most muscles are positioned vertically on the leg bones. In the foot, they run from the heel towards the toe joints, because most muscle send their tendons towards the forefoot and toes. The end of the toes and fingers do not have any deep fascia to help improve ‘finer’ gripping actions, but its absence increases the risk of bone infections after penetrating injuries.
Although up-down fibre orientation dominates in the lower limb’s deep fascia, many fibres run horizontally around the leg to create compressive loops that resist tissue expansion as the contracting muscles expand. Imagine wearing a tight elastic/Lycra wetsuit under your skin that tightens when muscles contract and expand, compressing the body tissues beneath. This gives you an idea of how fascia works by squeezing and pulling body parts together. It is also full of nerve endings so that fascia helps the body subconsciously know where everything is and how stably it is held together during motion.
Tensional forces caused by muscles contracting and joints moving beneath it, tighten fascia. This results from deep fascia being directly bonded to each muscle’s own fascial covering (epimysium). Some muscle fibres attach directly to areas of surrounding deep fascia, pulling directly on fascia during contraction. As a result, a significant amount of muscle force is transferred into and across fascia as well as the tendons and ligaments, before reaching the bones to create motion and stability.
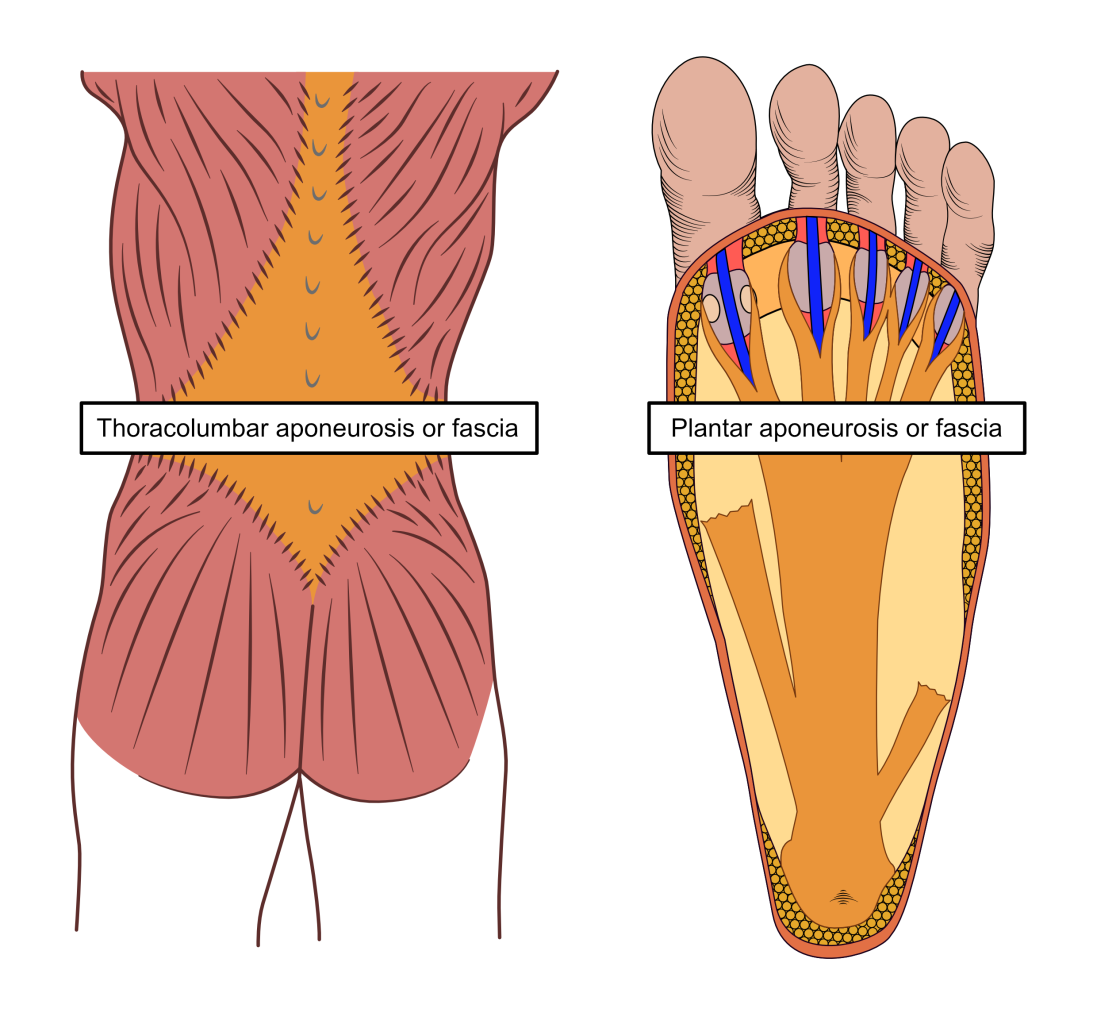
Fascia is thickened around joints like the hip, knee, ankle, and toes, but also in other specific areas where forces concentrate over the muscles beneath. Some areas of deep fascia experience higher forces in only one direction of tension. The deep fascia responds to this extra unidirectional stress during growth by arranging fibres in these areas to align to resist the repeated high tensional forces. These areas also thicken up. There are many of these thickened areas found across deep fascia. They are known as aponeuroses or retinaculum. The most well-known are the thoracolumbar aponeurosis or fascia that is found over human backs between the shoulder and buttock muscles, the iliotibial tract or band in the outside of the thigh, and the plantar aponeurosis or fascia under the foot. It is damage to the plantar fascia lying between the heel and toe joints that causes plantar fasciitis. To see three of the important fascial reinforcements of the body, see Figs 4 and 5.
Figure 3. Deep fascia fibres in the leg are primarily orientated in an up-and-down direction, with others forming rings around the leg as shown in the right image. When leg muscles contract, the up-down fibres of the deep fascia tighten while their expansion is restricted by the ring-orientated fibre. This tensions everything together tightly, especially in areas of reinforcement. There is a reinforced area in the outside of the thigh that uses tension forces generated by big hip muscles like gluteus maximus, to help stabilise the knee. This is the iliotibial tract or band, an aponeurosis that is often irritated during running.
Figure 5. Other deep fascial reinforcements (aponeurosis) are found in the back (left) and under the foot (right) in areas where fascia is loaded with lots of force. These provide strong structures for muscles to attach to as well as acting as powerful springs to resist and assist certain motions.
The anatomy of the plantar fascia
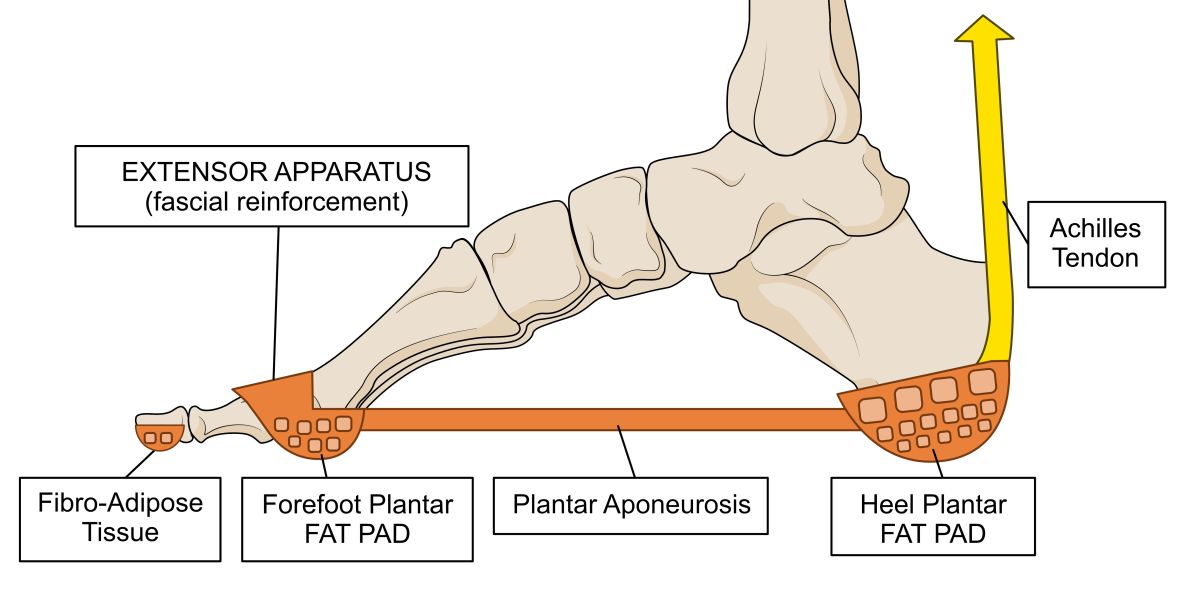
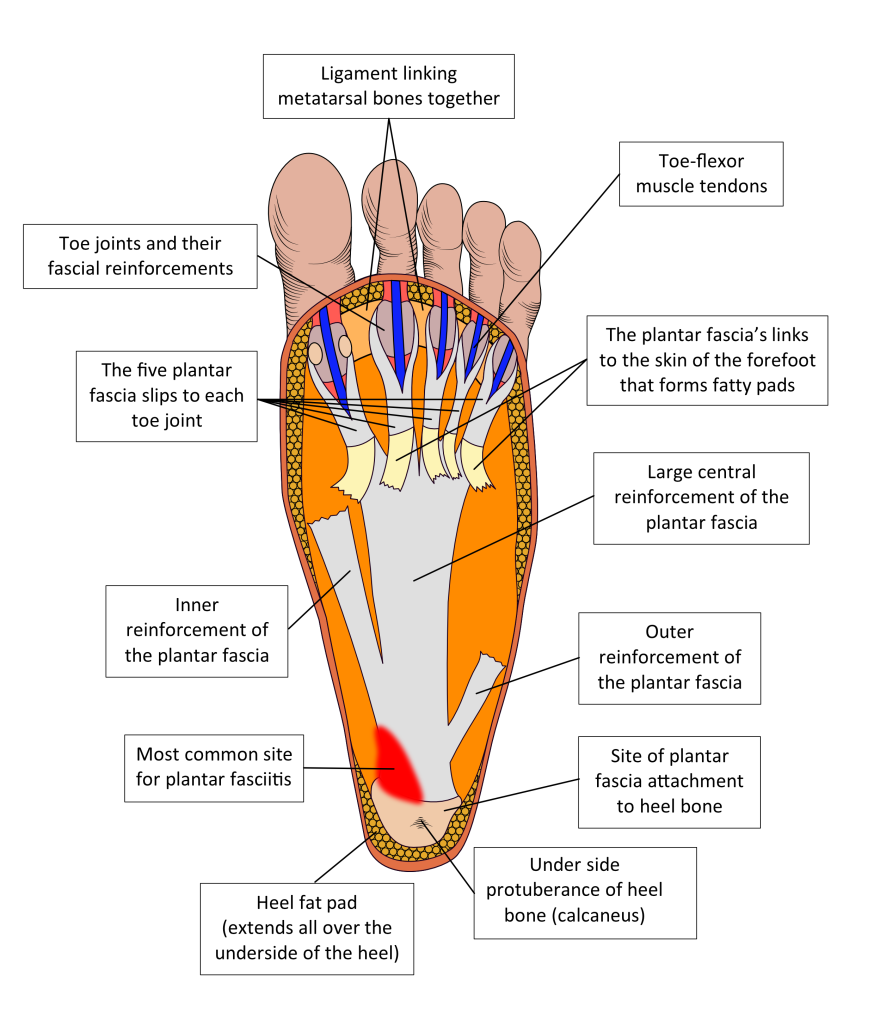
The thickened plantar fascia sits under the foot’s bones and muscles beneath the skin, binding the heel to the forefoot and toes across the length and width of the arch of the foot. There is no superficial fascia between the skin and the plantar fascia as there is elsewhere. Instead, the skin tissues bind directly to the plantar fascia. The presence of the tough plantar fascia makes the skin on the sole less flexible than in other areas of the foot, which helps prevent too much friction and shear against the ground. To further protect the skin and the forefoot weight-bearing surfaces, the deep fascia forms thousands of small chambers of fat over the heel and forefoot. These are the heel and forefoot plantar fat pads that act as shock absorbers and reduce pressure. See Fig. 6.
Figure 6. The plantar fascia links directly into special areas of deep fascia that form chambers of fat, acting as padding under the foot. If the fascia fails to hold the fat within the chambers, the padding in these areas is lost. This can cause both plantar heel pain and/or forefoot pains, depending on where the fat pads fail.
Failure of the fascial chamber walls allows the fat to squash down too much when weight-bearing, like worn-out foam padding. This is another common cause of weight-bearing plantar heel pain and/or forefoot pain (metatarsalgia). It tends to be noticed especially when wearing thin or hard-soled shoes. Unlike plantar fasciitis, it hurts the more time you spend on your feet, rather than mostly when first getting moving. However, having plantar fasciitis does cause deterioration in the mechanical properties of the heel fat pad.
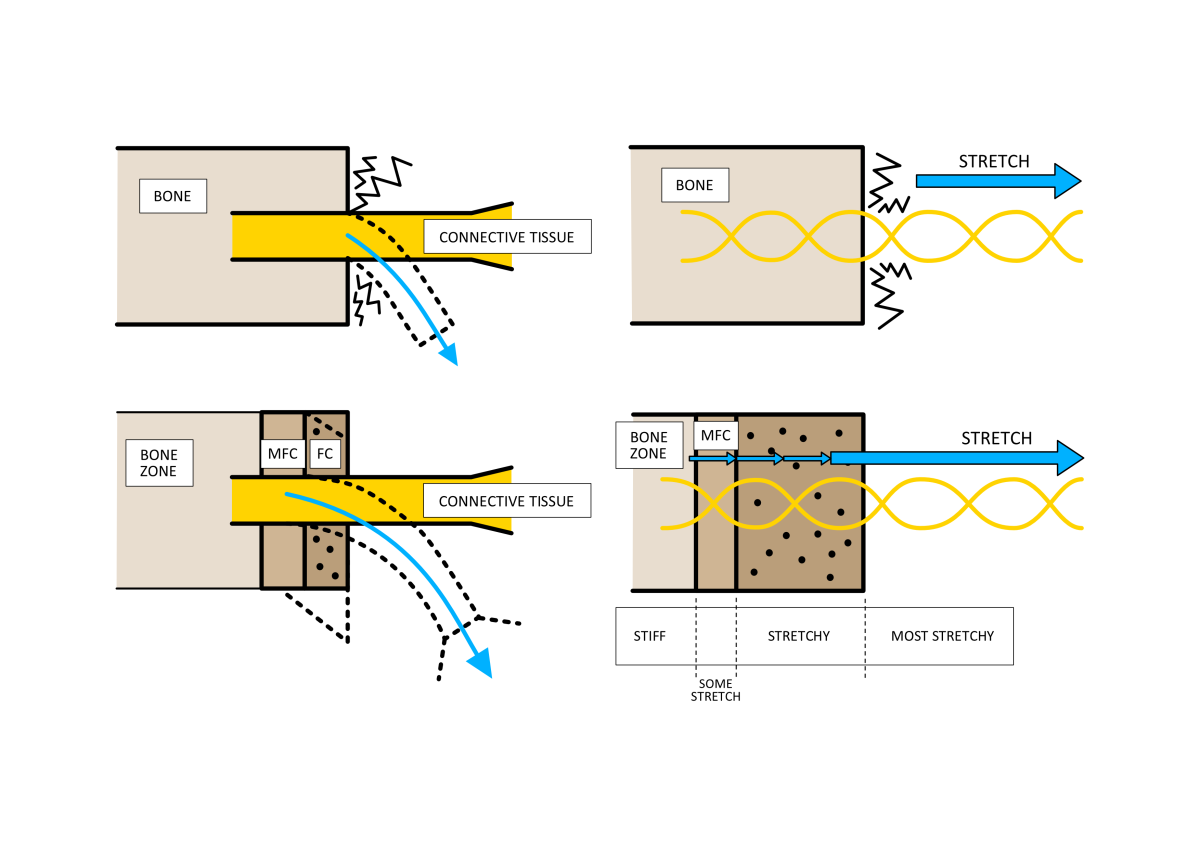
The plantar aponeurosis directly binds to the under (plantar) surface of the heel bone, where a large rounded protrusion forms the familiar shape of the underside of the heel. The heel fat sits over the prominent area of the heel bone that impacts the ground. The plantar fascia attaches to the heel bone and the fat pad, most extensively along the front (anterior) edge of the heel bone’s protrusion. These fascial binding points are similar to those formed by tendons and ligaments to bone and are known as entheses. The attachment areas are quite complex structures that consist of a graduated bonding of more flexible and spring-like collagen fibres to become mineralised stiff fibres that make bone hard. The gradual change in fibre stiffness prevents flexible fibres from bonding directly to solid inflexible bone fibres to avoid areas of high stress forming, as shown in Fig 7. However, this graduation can be disturbed, and this is something we will return to later.
Figure 7. Tissues such as fascia, ligaments, and tendons join bone through areas of mineralised fibrocartilage (MFC) and fibrocartilage (FC). The first benefit is that MFC and FC can like the grommet on a plug, a structure which protects the point of entry of the electric wire by allowing motion without damage. Compare the upper left image without MCF and FC to the lower left image. The other benefit is that when connective tissue tension on bone, any strain will not concentrate on the stiff/flexible interface between the bone and the stretchy connective tissue fibres. Compare the upper right image to the lower right image.
Most plantar fascia fibres run from the heel attachments towards the toes. However, some run forward towards the sides of the foot to blend with thinner areas of deep fascia that cross around and over the top of the foot and around the ankle (where it is also reinforced). Some plantar fascia fibres also run deep into the foot to form connective tissue walls that muscles under the foot can bind to. These penetrating fibres eventually bind into the ligaments and fascia covering (periosteum) on the underside of the foot bones. In the forefoot, other sheets of fibres run superficially as they progress forward to bond to the undersurface of areas of the skin. These skin-slips trap fat to form the forefoot fat pads that protect the bones within the ball of the foot.
However, the bulk of the plantar fascia fibres run under the arch, forming a thick central band that finally splits into five slips. Each slip runs to each toe joint. Here the plantar fascia binds to the ligaments that link the metatarsal bones together at the toe joints. These distal attachments play a very important part in keeping the joints stable. This linkage is particularly important as we accelerate forward on the forefoot after the heel lifts off the ground.
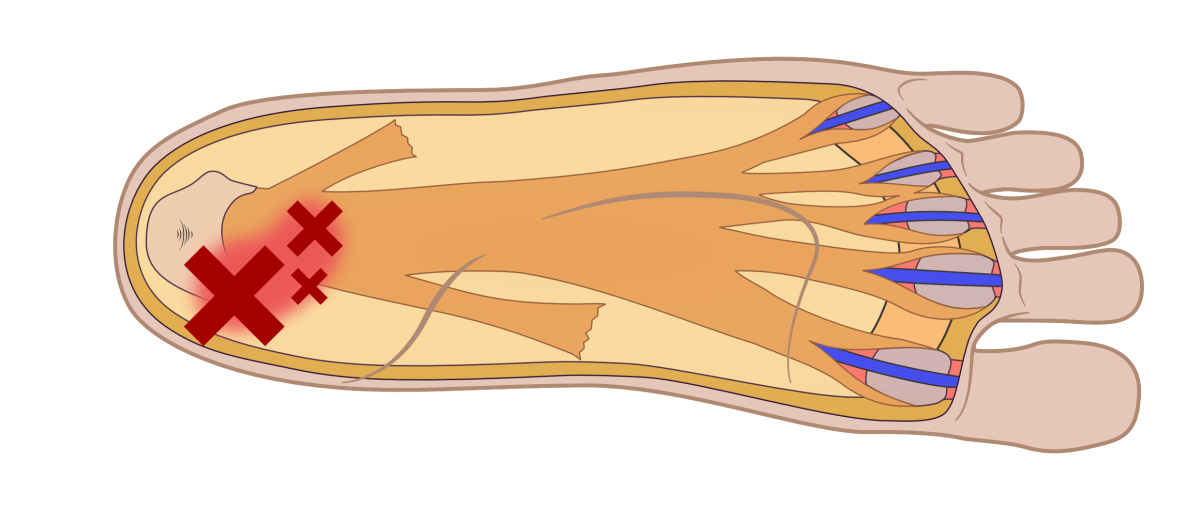
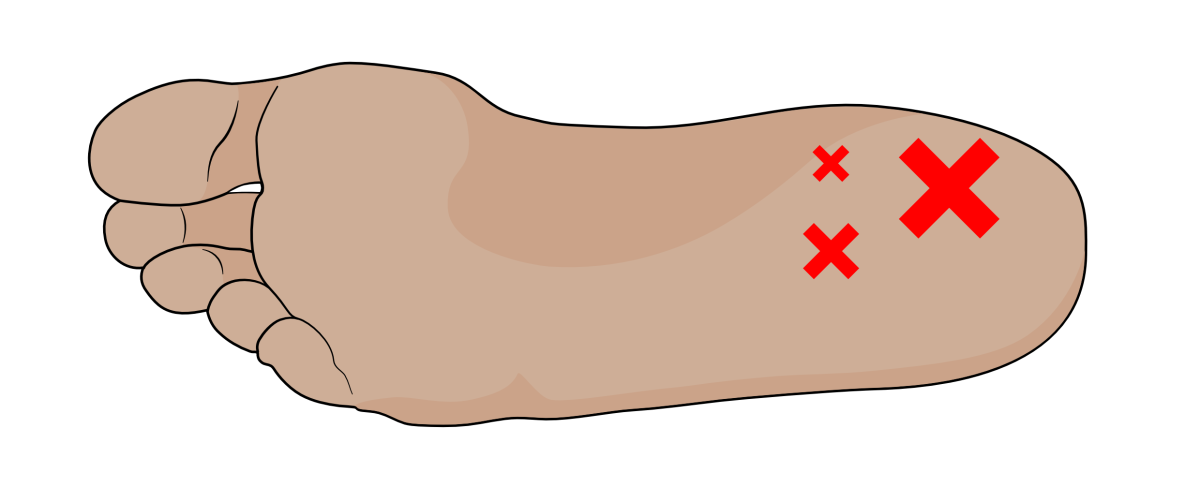
Because the arch of the foot is higher and changes in height mostly on the inside of the foot, greatest tension forces occur along the inner edge of the central band of the plantar fascia, just where it attaches to the heel. Thus, this is the most common site of plantar fasciitis. See Fig. 8 for a rough guide to the plantar fascia’s anatomy and the most common site for plantar fasciitis.
Figure 8. The plantar fascia as viewed from under the foot with the skin and plantar fat pads removed. The slips that link to the skin in the forefoot area have been ‘pulled’ backwards to show the important deeper fibres running to the toe joints. In life, the slips to the skin run towards the toe areas, enclosing pockets of fat to provide forefoot cushioning.
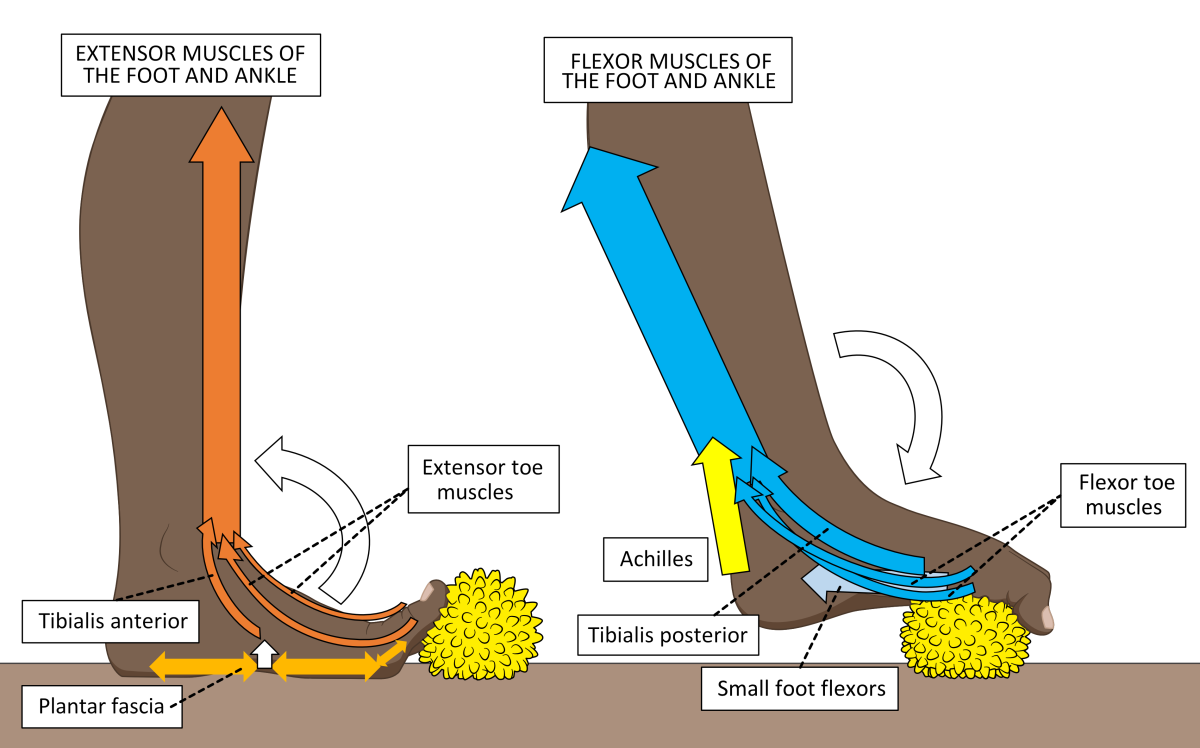
By reinforcing the heel to the toe joints, coupled with complex attachments connecting to pretty much all the anatomy under the foot, the plantar fascia offers around 25% of the forces that bind and stiffen the underside of the foot. It is like having a tightly bound sole-less moccasin under your foot. The greatest influence on binding the fascia tight are the forces generated by the muscles of the foot, aided by deep ligaments binding the foot bones together. Supporting muscle forces derive from calf muscles and those muscles packed across the arch under the bones of the foot, as shown in Fig. 9.
Figure 9. Muscles of the lower leg and foot are shown exercising with a Healthy Step foot therapy ball. When the extensor muscles on the front of the shin pull upwards on the toes, the plantar fascia tensions across the foot’s arch (left image). However, it is the activity and strength of the calf’s flexor muscles (right image) and small foot flexor muscles found within the arch that have the greatest effects on the plantar fascia’s stability and tension during gait and standing.
The plantar fascia isn’t found in other large primates for it has evolved under the biomechanical forces generated by human’s distinct bipedal gait to enhance the mechanical efficiency of the foot. Its presence allows the use of less muscle power to stabilise the foot during walking.
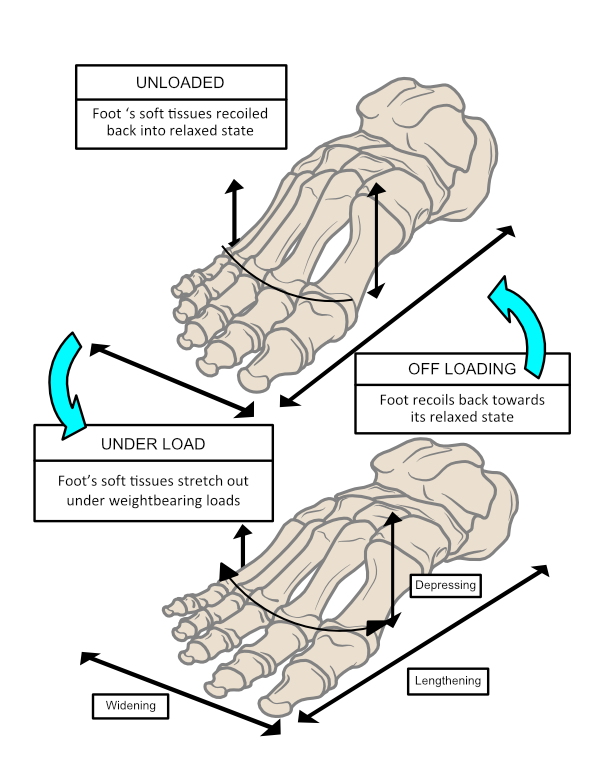
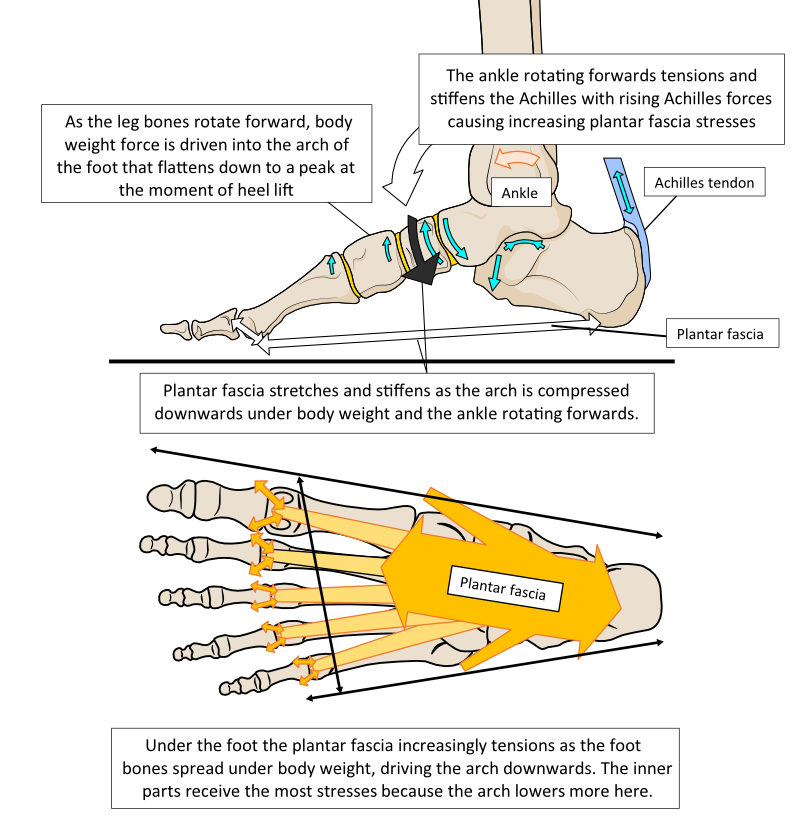
A rough guide to effective foot function
During a step, the heel usually makes contact with the ground first followed by the forefoot. This distinct two-part impact occurs because the foot has an arch separating the heel from the forefoot. Once the forefoot contacts the ground, all the body weight is loaded onto one foot as the opposite leg and foot start to swing forward. The arch is now permitted to quickly flatten elastically to allow it to act as a shock absorber. The plantar fascia is one of the structures that elastically tension under the foot as the arch flattens to provide this shock absorption. Flattening the foot creates tensions across all the soft tissues under the foot bones, many of which the plantar fascia has direct and indirect attachments to. The elastic tension provided limits the rate and amount the foot can lengthen and widen.
Foot flattening not only allows shock absorption but also increases the sole’s surface area in contact with the ground. The effect of increasing the contact surface area is to lower the peak pressures generated on the sole of the foot. Pressure is force over an area. With more area in contact, forces can spread out to reduce the peak pressures on tissues under the foot. Thus, dynamic spring-loaded foot-flattening helps avoid damaging the skin and deeper tissues beneath it. As body weight forces unload at the end of the weight-bearing phase as the heel lifts, the foot can spring back into shape as shown in Fig. 10.
Figure 10. The foot acts as an elastic shock absorber, squashing down under load and then springing back into shape once off-loaded. The plantar fascia plays a significant part in this mechanism being maximally tensioned, lengthened, and full of elastic recoil energy as the heel starts to lift from the ground.
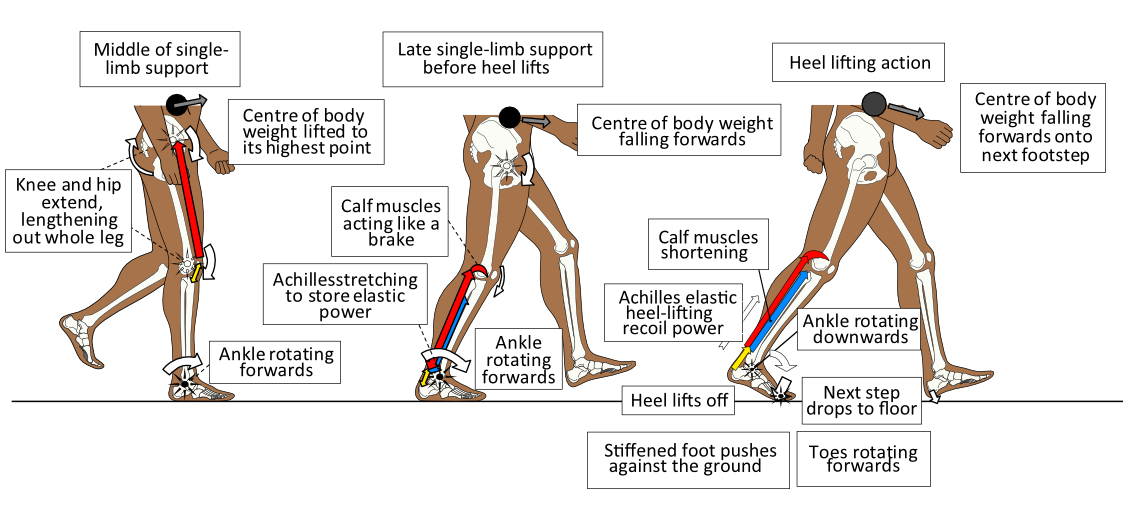
The power to lift the heel off the ground towards the end of a step arises primarily from the stretched Achilles tendon recoil. The strong Achilles is stretched as the ankle rotates forward with the body passing above and over the single supporting foot in the second half of the foot weight-bearing phase. The Achilles tendon should be so full of elastic power towards the end of a footstep, that it wants to pull the heel away from the ground. This becomes easier as body weight moves away from the heel towards the forefoot, reducing forces that keep the heel on the ground. To achieve an efficient heel lift, the foot needs to be semi-stiffened so that the forefoot can more easily push against the ground as the heel lifts. A flexible foot at this time will cause foot buckling in its middle, an event known as a ‘midfoot break’.
The action of flattening the weight-bearing foot that stretches ligaments, tendons, and fascia, and by also activating muscles under the foot, supplies the foot with adjustable stiffening abilities. With a stiffer foot, Achilles tendon recoil power can lift the heel and force the ankle to rotate downwards and forward easily, pivoting the foot over the big (1st), 2nd, and 3rd toe joints as shown in Fig. 11. This is the most mechanically efficient way to use the foot in locomotion.
Figure 11. After the leg has functionally lengthened by extending the hip and knee during the first part of the single limb supporting period, the foot increasingly stiffens. Ankle rotation is slowed by calf muscle power as body weight (black spot) falls forward. This action stretches and tensions the Achilles elastically. Once body weight has moved over the forefoot, the heel ‘pops up’ off the ground under the recoil power of the Achilles, rotating the rearfoot upwards and forwards over the forefoot and toe joints.
Thus, it is the calf and foot muscles that primarily control the rate of foot flattening and stiffening during each step. However, the muscle-induced control of the foot’s flexibility is improved by healthy ligaments and fascia. Adaptability in muscle-induced stiffness is necessary because different surfaces require different degrees of foot flexibility during each step. A permanently solid or floppy foot could not provide such necessary variability. Therefore, appropriate foot flattening controls foot pressures and provides stretching tensions on ligaments, tendons, and fascia. This allows the foot to act as both a shock absorber and a recoiling spring. Elastic power released under the foot at heel lift ‘recoils’ the foot back into shape after heel lift. Controlling stiffness across the arch appropriately avoids ligament, tendon, fascia, muscle, and joint damage that could result if the foot squashes down too much or insufficiently.
That’s basically how a foot works!
What does the plantar fascia do?
The plantar fascia has important roles in shock absorption, the ability to stiffen the foot, and in managing forces across the foot. Its restraining and elastic properties provide shock absorption and energy dissipation that is generated when impacting the ground and as body weight passes over the foot. It also assists in managing the Achilles-generated power applied across the foot, especially at heel lift. If too high, these forces could cause injury but if too low mechanical efficiency of walking is reduced. Human feet can work without the plantar fascia, but its presence makes walking more efficient and less tiring. This is why the plantar fascia has evolved as a response to biomechanical forces generated by human’s unique form of walking.
Simply put, once you have a long, thick, and very powerful Achilles tendon controlling body motion set high up on high legs passing over the foot, a thick plantar fascia is beneficial. The elastically tensioned Achilles produces a powerful heel-lifting action using a long, narrow foot that pivots at forefoot joints with short toes. This causes humans to generate forces that reorganise the foot’s deep fascial development. Once walking has started during infancy, the forces from the Achilles and the toes bending upwards cause the deep fascia to form into a highly organised thickened area of semi-elastic fibrous tissue with fibres running from the heel to the toes. As we grow taller and become heavier, the fascia gets stronger to cope with the higher stresses.
Thus, the plantar fascia can act as a mechanism to link Achilles tendon forces to toe joint motion and forefoot stability. This is highly advantageous because the correct level of flexibility of motion at the toe joints is linked to how stable the forefoot is and how much stress is put on the Achilles. This relationship also directly affects loading forces on the other foot’s heel contact. Too much or too little foot flexibility without adaptability will be a problem. Many leg and foot muscles are involved in setting this adaptability. By having a strong, thin semi-elastic band under the skin running from the heel to the toe joints, controlling the level of foot stiffness becomes much easier for the muscles. See Fig. 12.
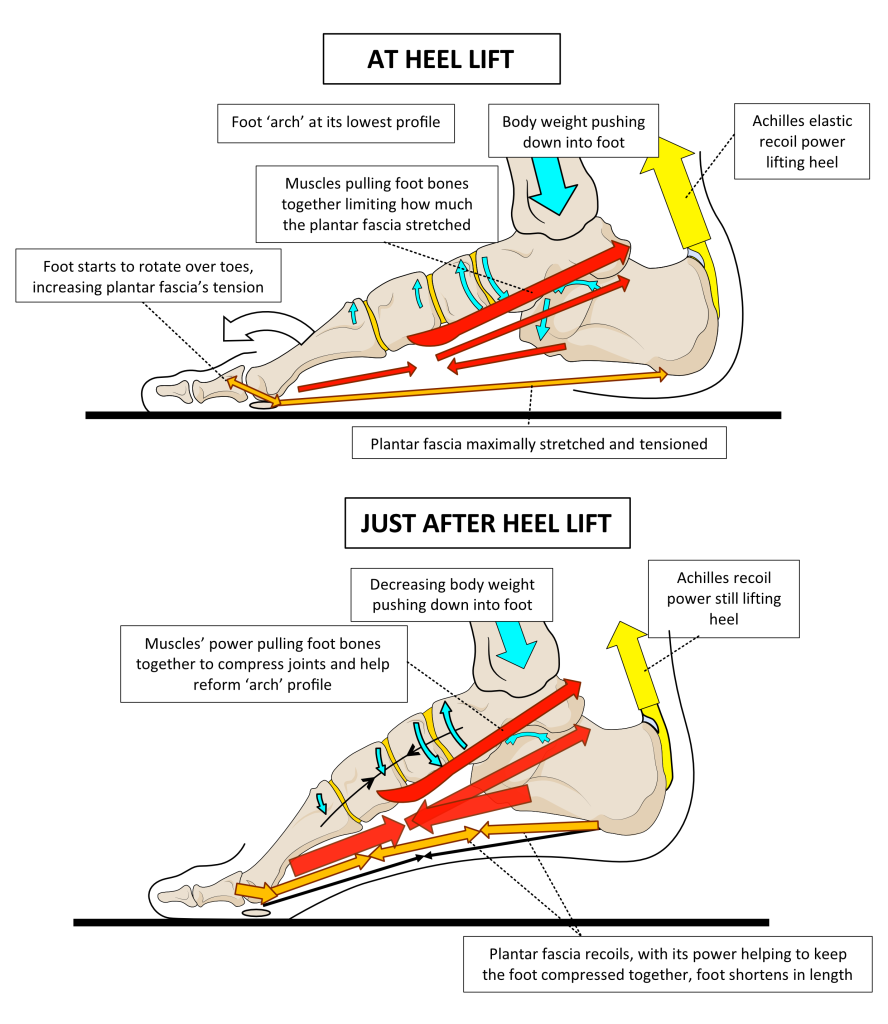
Figure 12. At the moment of heel lift, the foot is at its lowest profile and the plantar fascia is at its highest tensional stress. After heel lift, when most of the body weight has moved to the next footstep, the plantar fascia works with the elastic recoil power of tendons under the foot to spring the foot back into a shorter, higher-profiled shape.
Power generated by the muscles that supply the foot helps limit the stresses placed on the plantar fascia by compressing the foot together. This action prevents the foot buckling in the middle under the heel-lifting power of the Achilles. After heel lift, stresses on the plantar fascia start to drop and it now recoils to shorten with the foot as its ‘arch’ profile starts to rise. Tendon elastic recoil power from the muscles under the foot assists in this stable recontouring, despite the muscles relaxing at this time. When walking, most body weight should be transferred to the opposite foot just after the heel lifts. This rapidly reduces stress on this foot, allowing muscles to relax and permitting the foot to spring back into a higher profile under elastic recoil alone. This is an action that the plantar fascia plays an important part in.
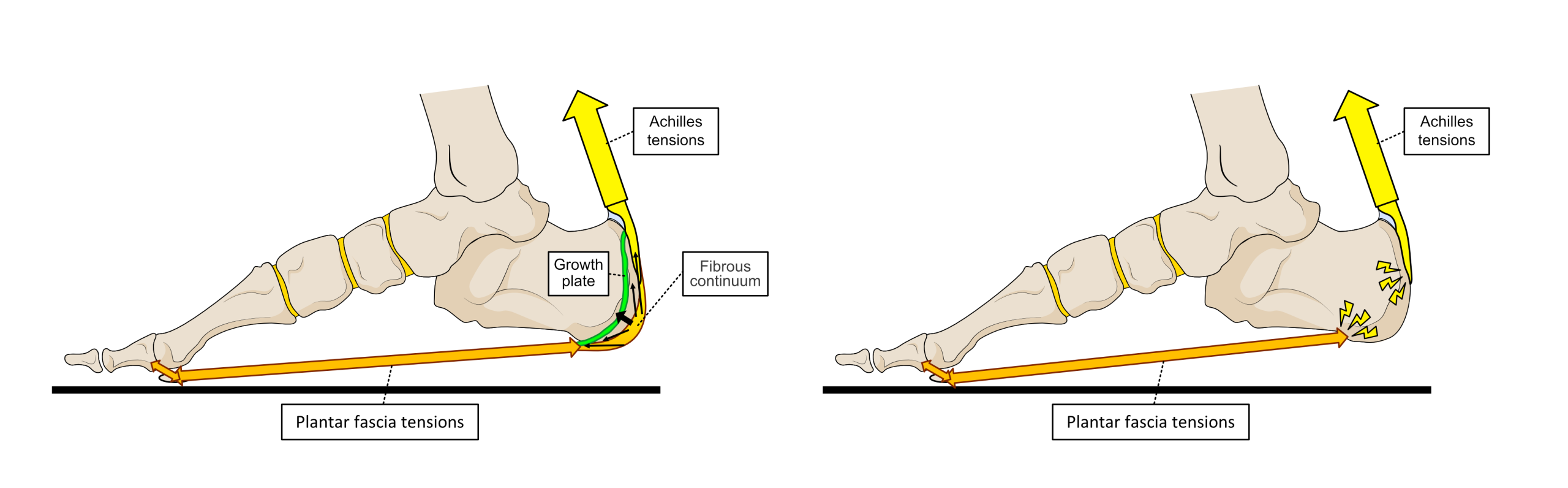
The fact that the Achilles attaches to the back of the heel bone and the plantar fascia to the underside of the same bone, links together the motion of the heel bone to the level of tension in both the Achilles and the plantar fascia. During foot-flat weight-bearing, forces applied by the Achilles tensioning into the back of the heel bone have a direct relationship to rising stresses within the plantar fascia. Until humans are mature, fibres from the Achilles tendon not only attach to the back of the heel bone but run around and under the back of it to blend into the plantar fascia. Quite why these connecting fibres are lost and only the strong bone attachments remain as humans age is unclear. However, it does mean that the heel bone-fibrous attachment points become areas of higher tensional forces in mature humans compared to younger ones. See Fig. 13.
Figure 13. Until full maturity (left image), fibres run between the Achilles tendon and plantar fascia that form a fibrous continuum over the heel bone. This allows stresses to run directly between them as well as at their heel bone attachment points. While the heel bone is growing, a growth plate of fibrocartilage (green area) separates the heel bone into two bone areas. Under tension and compression caused by the Achilles and plantar fascia activity on the growth plate, the back of the heel bone forms the correct shape for the individual. However, excess stresses here can provoke pain in 9 to 13-year-olds. The right image shows the mature situation, where tension on the Achilles and plantar fascia are all directed into their bone attachment points alone. This is possibly why plantar fasciitis is only a problem seen in mature humans.
An obvious conclusion from this Achilles-plantar fascia relationship is that heavier people with tight calf muscles have a potential risk of tensional forces exceeding the plantar fascia’s capacity, especially at the heel bone attachment. However, there are many other risks to the plantar fascia becoming over-strained, especially as humans age.
The plantar fascia’s role in supporting the arch
As already stated, the plantar fascia is important in shock-absorbing under walking and running forces and also in aiding foot stiffening before forefoot contact and after heel lift. It achieves these tasks through the foot possessing a 3-dimensional vaulted or domed profile under the middle of the foot, commonly known as the ‘arch’. The arch offers the foot many advantages, including the ability to deform and flatten, tensioning the soft tissues to give the foot spring-like shock-absorbing properties.
As the foot flattens by lengthening and widening under body weight, the elastic connective tissue structures of tendons, ligaments, and fascia stretch and stiffen between the bones. Stretching helps shock absorption, while stiffness permits some recoil energy to be stored within these tissues. This makes the foot increasingly stiffer and elastic as it flattens to its lowest profile just before heel lift. Stiffening the foot by stretching it, makes it easy for muscles to create a more stable structure to aid heel lift. A stiffer foot means most motion can only occur at the more flexible toe joints. Thus, the whole foot lifts as one by rotating on the forefoot at the toe joints under the power released from the Achilles.
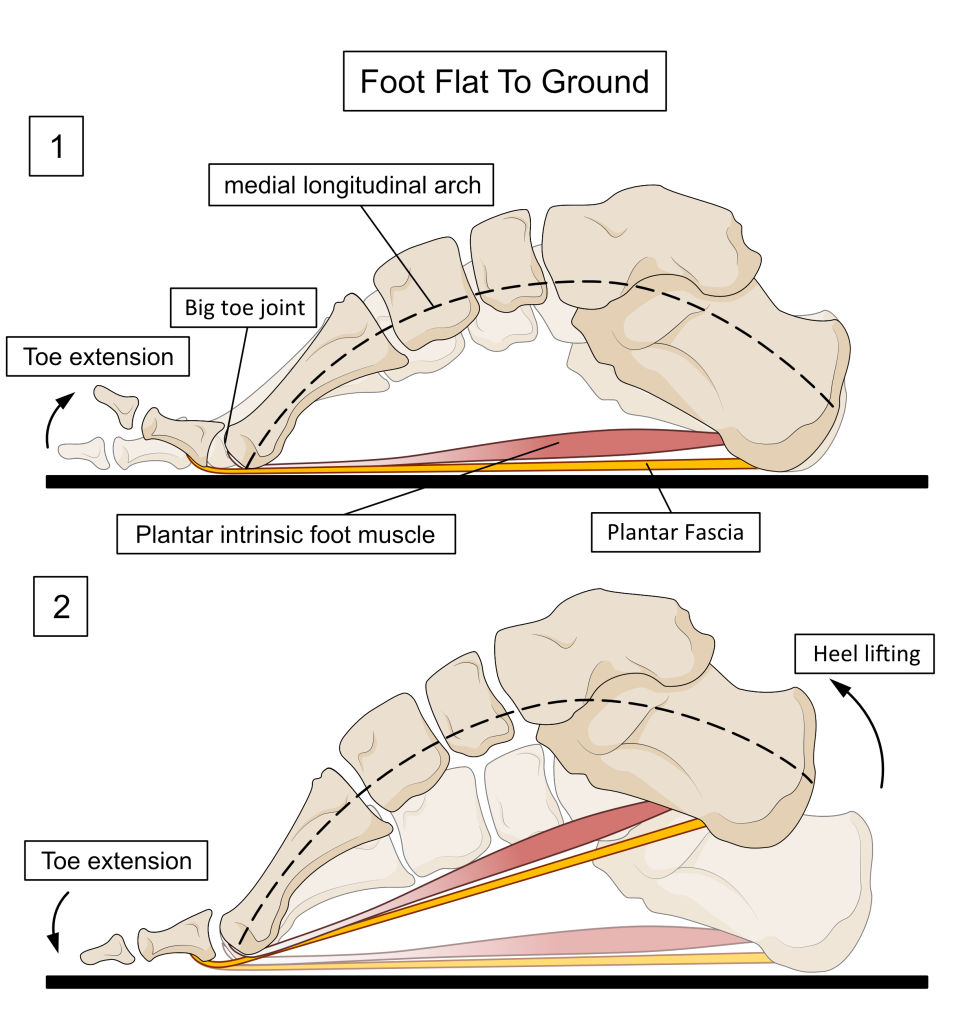
The reason the plantar fascia can stiffen the foot is down to the fact that it attaches to the most proximal toe bone across the toe joints found at the ends of the long forefoot bones, called metatarsals. When toes are bent upwards, the plantar fascia tightens the foot across the arch elastically, which means it is a sort of spongy tightness rather than a rigid stiffening. This effect can be felt easily on a non-weight-bearing foot with a finger placed under the arch. When pulling the toes upwards you will feel and often see the plantar fascia tighten under the foot.
When walking, the effect of extension of the toes is a little different because when the foot is flat on the ground, the toes should never extend upwards. However, the principle of winding the plantar fascia around the metatarsal head using upward-rotating toes to tension it, does occur before forefoot contact and after the heel lifts. This action has been referred to as being much like a ‘windlass’ used to tighten ropes in sailing etc. Thus, raising tensions of the plantar fascia by rotating toes upwards is called the ‘windlass effect’, while allowing the toes to move downwards reducing fascial tension, is known as the ‘reverse windlass effect’.
When the windlass effect occurs, the plantar fascia tightens and the distance between the heel and the toe joints shortens, causing the arch of the foot to rise. During reverse windlass effects, the tension on the plantar fascia reduces and the foot can more easily lengthen and widen to lower the arch. Because the metatarsal bones toe joint end (head) is bigger at the big toe joint, and because the second metatarsal next to it is usually the longest, stresses through the windlass mechanism are greatest on the plantar fascia that is bridging the inside of the foot arch. The inside of the foot also changes its height the most and as a result of these factors, higher stresses occur around the inner edge of the fascial attachment to the heel bone.
By pulling the toes upwards before forefoot ground contact, the windlass effect pulls the plantar aponeurosis tight. This stiffens the foot and shortens the arch, making the foot more elastic and spring-like. Like this, the foot makes a better shock absorber when the forefoot collides with the ground. At forefoot impact, the toes relax to allow the windlass mechanism to reverse. The toes can now rotate downwards under forefoot impact forces to create a more flexible foot. In this manner, the foot can now dissipate impact forces by acting more like a deforming cushion. The windlass mechanism is only initiated again after heel lift as the toes are forced to extend upwards by the rest of the foot rotating over the toes. This allows the arch to rise again and the foot to remain stable, despite muscle activity decreasing after heel lift. This latter plantar fascia stiffening action lasts almost until it is time to remove the toes from the ground to complete a step. See Figure 14 to see how the windlass works by bending the big toe up or via lifting the heel over the toes.
Figure 15. When the foot is flat on the floor, pulling the toe upwards into extension tightens the plantar fascia, shortening the foot and raising the arch as shown in image 1. In walking, this ‘windlass’ action occurs before forefoot contact and reverses as the forefoot strikes the ground. This ‘reverse windlass’ allows the arch to lower and the foot to lengthen. Toes extend the most after heel lift as the foot rotates over the forefoot, activating the windlass mechanism again as shown in image 2.
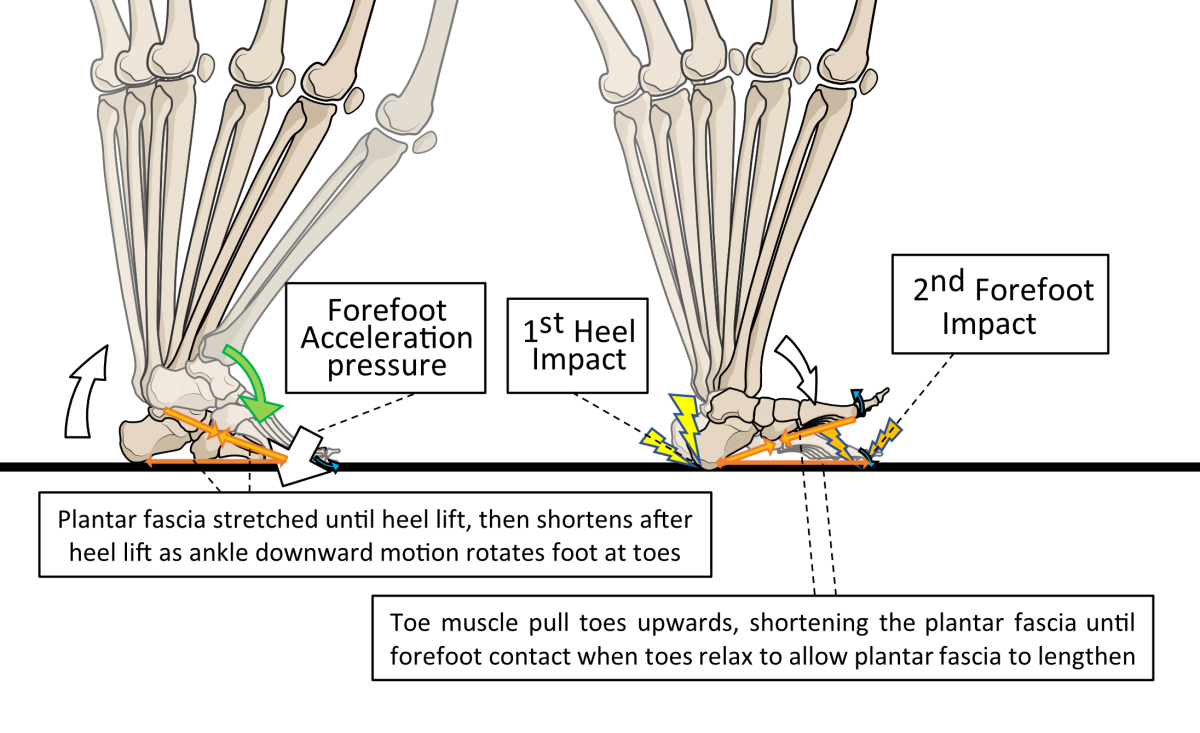
The windlass mechanism is first initiated because the toes pull upwards when the muscles on the front of the shin are breaking downward ankle rotation caused by heel strike. These muscles control the speed at which the forefoot hits the ground. Using the windlass mechanism before forefoot contact helps stabilise and increase the vault profile, enhancing the distinctiveness of the heel and forefoot areas. This allows the foot to hit the ground twice, first via a heel impact followed a little later by a separate forefoot collision. Such an approach divides the collision forces of ground contact into two smaller-force events rather than having a single bigger impact. Thus, tightening and shortening and then relaxing the arch profile, allows the plantar fascia to influence contact impact shock-absorption. By retightening the arch again after heel lift, the plantar fascia assists foot stability during acceleration and we move forward towards the next step, as shown in Fig. 15.
Figure 15. Collision forces are applied to the forefoot pushing downwards under heel-lifting power from the Achilles (shown for the right foot), as the opposite foot (left foot) makes its initial ground contact. By first hitting the ground via the heel and then the forefoot, the foot divides impact into two lower collision forces rather than one big impact. For this process to work properly, the plantar fascia must tighten before the forefoot makes contact and after the heel lifts. The plantar fascia uses a mechanism of winding its fibres under toe joints to tighten or loosen it, so that toe positions and motions as well as muscle strength, are important for plantar fascia function.
Thus, as one foot tightens its plantar fascia after heel lift the other tightens before forefoot contact. Once the forefoot hits the ground, the windlass mechanism is reversed which causes the toes to rotate downwards, taking tension off the plantar fascia to absorb impact forces through the arch lowering and by foot lengthening deformation. After this, the plantar fascia gradually tightens as it stretches through body weight moving forward over the foot by ankle rotation. The foot lengthens and widens. Greatest length changes occur across the inside edge of the foot so stresses and strains tend to concentrate on the inside edge of the plantar fascia. See Fig. 16.
Figure 16. The foot lengthens and widens under body weight forces, stretching and tensioning the plantar fascia. Deformation of all the soft tissues under the foot acts as a shock absorber. The plantar fascia plays an important role in this. Plantar fascial tensional stresses reach a peak as the ankle rotates forward as far as it can before the heel lifts from the ground. The highest stresses are experienced where fascia connects to bone tissue, especially around the inside heel area.
When the heel lifts, the plantar fascia is still stretching/lengthening helping to stiffen the foot. However, this drives large stresses across the plantar fascia, especially at its bony attachments to the heel.
What is plantar fasciitis (or plantar fasciopathy)?
The name ‘plantar fasciitis’ means ‘fascial inflammation’. However, it is caused by a chronic overstraining of the plantar fascia that causes repeated damage around its attachment site to the heel bone, especially on the inside of the foot. See Fig. 17.
Figure 17. ‘X marks the spots’ where most cases of plantar fasciitis occur. The larger the X, the more likely the pain will peak within that area.
The resulting damage causes a combination of low-grade inflammation and degeneration of the plantar fascia. There is also a build-up of inflammatory fluid within the surrounding heel bone. This is why experts on the foot tend to call the condition plantar fasciopathy (‘fascial pathology’) rather than fasciitis to reflect that it is just as much a degenerative process as an inflammatory one.
When body tissues are damaged, they attempt to repair, which requires the complex process of inflammation to start the process. Inflammatory fluid contains chemicals that cause pain and sensitivity to the copious nerves found within the fascia. This is most noticeable when fibres are first strained when standing down and starting to walk. Walking itself starts to pump some fluid out of this area of the foot, which reduces the pain. This is why plantar fasciitis symptoms are worse when first loading the affected foot after resting/sleeping. Pain is a ‘warning signal’ that alerts the body that some part of it requires protection.
If repair is quick, the heel pain symptoms won’t last too long or be very noticeable and the fascia will reform a little thicker than it was previous to increase its strength. Reducing the stress on an injured area speeds up healing. The problem for any injury within the foot is because of the need to keep walking, taking the stress off it is far more difficult than in, for example, the arm or hand. Plantar fascia receives a lot of stress throughout every step and it is even under strain when just standing. Its stresses are greatest around the moment of heel lift because the plantar fascia is at its longest length and thus at its greatest strain at that moment and just after. However, once injured it requires far lower stresses than normal to cause further damage to the weakened tissue. If the rate of foot-loading forces damaging fascial fibres outstrips the rate of healing or even just matches it, a chronic cycle of degeneration and attempted healing sets up, causing long-term problems.
Most people who seek help with their plantar fasciitis are caught in this cycle of chronic healing and re-damage.
What happens as a result of plantar fasciitis?
When attempting to heal, tissues require increased blood flow to bring in all the substances necessary to construct new tissue. This causes inflammation that results in swelling (oedema) which heightens nerve sensitivity. Pain sensitivity acts as a warning to get stresses off an area while it is healing. Inflammation stops once the repair is made. Then slowly pain and swelling will go away as further healing processes help the tissues to remodel to improve strength. There is a mechanical weak point where plantar fascia and bone meet, which makes it far more likely for it to be injured at the heel. Indeed, the plantar fascia can often be injured (torn) in other areas of the foot, but the symptoms and the causes are quite different and should not be called plantar fasciitis.
The problem for the plantar fascia is where the elastic properties of the fascial fibres bind into the stiff, largely inflexible fibres of the heel bone. As previously mentioned, the join of these mechanical different fibres involves a very gradual change from elastic areas to regions of a little less elasticity, to transition zones of more stiffness before becoming very stiff bone fibres (see Fig. 7 again). This gradual change is achieved by adding increasing amounts of fibrocartilage around the normal connective tissue fibres and then increasing the amount of bone minerals within the fibrocartilage as it approaches the bone. Under tension, these fibrous unions show greater stretch (strain) the further they are from the bone and the least nearer to the bone, but in a very graduated manner. This gradual change in materials and compliance properties across the fibres can be disturbed by minor injuries to the area.
Sometimes, too much mineralisation occurs across the union site’s fibres. This results in new bone growth (ossification) into the fascia’s fibres. This process can be initiated by inflammatory or over-straining processes during attempted repair of a small injury within the area. These areas of new bone (seen on X-rays) are known as bone spurs or calcifications and those associated with the plantar fascia are called heel spurs. They are a sign of issues at the attachment, but they are not the cause of the plantar fasciitis pain for they are also seen in people with no history of heel pain. However, heel spurs indicate that repair processes have been taking place which could further concentrate forces on the attachment fibres of the plantar fascia. The presence of heel spurs in cases of plantar fasciitis seems to make the condition harder to resolve.
Why does plantar fasciitis happen?
Most cases of plantar fasciitis affect people in their 5th, 6th, and 7th decades of life. This is because human tissues start to degenerate in our forties. This means the ability to heal slows and tissues start to lose their ‘younger’ elasticity. However, most people remain quite active throughout their forties, fifties, and sixties, so the plantar fascia is still under a lot of mechanical strain. Thus, older but active adults are most at risk of developing plantar fasciitis with the incidence reducing once people reach their seventies when activity levels for most, start to reduce.
Thus, the simple cause of plantar fasciitis for most is their age combined with their activity levels. However, chronological age in years and tissue ageing do not always match across individuals. Certain lifestyles and health issues can cause plantar fasciitis to occur at far lower levels of activity and younger ages than in others. Certain diseases and habits (like smoking or poor diet) cause premature ageing of connective tissues. One of the most common of these diseases is diabetes which due to the presence of excess sugars in the blood, accelerates the ageing of connective tissues like tendons, ligaments, and fascia. This makes them stiffer, brittle, and thus more injury-prone.
The foot’s muscle strength is also very important in preventing plantar fasciitis. The plantar fascia relies on muscular activity under the foot to help manage the amount of stress applied to it. Some foot muscles bind directly to the deeper (or upper) surface of the plantar fascia, while all have indirect connections to it. Weaker foot muscles are less able to control the amount of strain put through the plantar fascia. Importantly, it has been found that people with plantar fasciitis have on average, less muscle bulk in the foot than those without. This supports a link between plantar fasciitis and poor muscle strength. Muscle mass is lost with reduced activity and takes time to rebuild, more so as humans get older. Therefore, those who are intermittently active, particularly those who have periods of low activity followed by very high activity, are most at risk. This is especially the case if you are an older adult. For example, mature hikers who tend to avoid the bad weather of winter but come out again for long walks in the spring may start to develop plantar fasciitis as the days get longer.
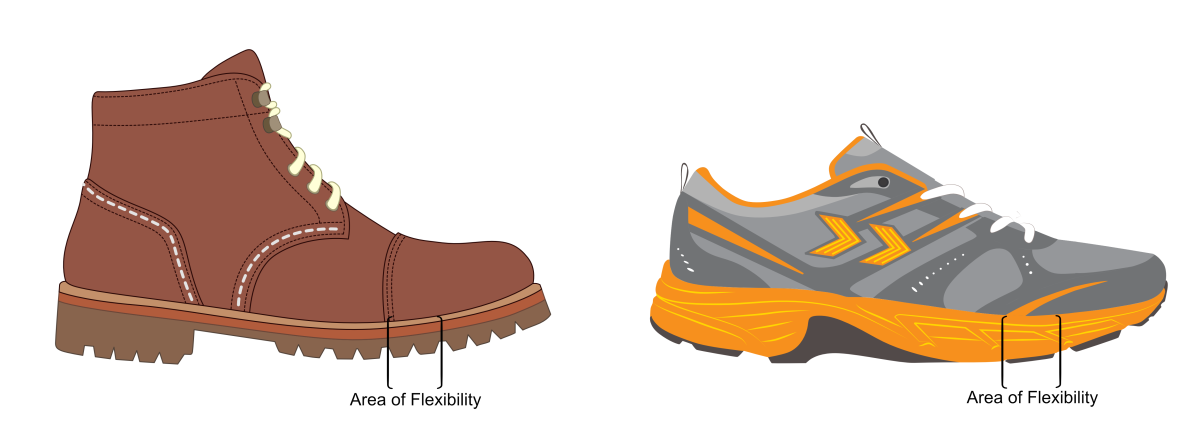
Other groups where having muscle strength sufficient to protect the plantar fascia is important are those who participate in highly active sports such as running. Again, older runners with weaker foot muscles are more at risk. However, suddenly increasing running distance, pace, and/or frequency may trigger plantar fasciitis. Using more flexible, less supportive running shoes without adequate foot strength may also trigger it. Generally, runners who develop plantar fasciitis are those with heavier builds, often in their thirties or early forties. However, the author has even seen several runners in their late twenties develop plantar fasciitis.
Muscle strength in the foot needs to match the amount of strain put on the feet. Lots of regular exercise requires stronger feet. However, the amount of strain placed on the feet also relates to the amount of body weight passing over them as well as the footwear worn. It is reported in the science that being significantly overweight increases the risk of developing worse and prolonged symptoms. Thus, being overweight but relatively inactive can also cause a mismatch in the foot’s muscle strength. The use of softer, flatter shoes that require foot muscles to work harder can also provoke issues. If muscle strength is required greater than that available, the plantar fascia is one of the foot structures that is going to experience more strain during weight-bearing activities, even just during standing.
It is important to note that the attachment point of the plantar fascia to the heel bone can become inflamed and painful for reasons other than mechanical overstrain. Certain autoimmune conditions also cause plantar heel pain via damage to the plantar fascia attachment. The most common condition for causing this is psoriatic arthritis. It has this name because it is far more common if you have symptoms of psoriasis affecting the skin or particularly your nails, or if you have other close genetic relatives with psoriasis. However, you can have psoriatic arthritis without any history of psoriasis. Autoimmune diseases are a result of the cells that fight infection attacking normal body tissues by mistake. Onset relates to genes and lifestyle events that trigger a misfiring of the immune system. Provocation includes having a nasty illness, particularly bad viral infections. In the case of autoimmune diseases such as psoriatic arthritis, ankylosing spondylitis, and Reiter’s syndrome it is the cells of connective tissue attachments that are mistaken for something foreign. Many different sites can be attacked, including around the toes and the Achilles tendon’s attachment. However, if the plantar fascia’s attachment is attacked first, a diagnosis of mechanical plantar fasciitis can be made by mistake. These problems (known as enthesitis) require pharmacological and lifestyle management. Although the treatments for plantar fasciitis may help symptoms, you will need to see a rheumatologist.
One final important comment is that children are not normally affected by plantar fasciitis. This is because plantar fasciitis is a degenerative issue. Children are prone to a form of heel pain on or after activity. This is a result of Sever’s disease or syndrome. This is a symptom related to the amount of strain placed on the growing heel bone and is far more common in children frequently playing multi-directional sports such as soccer, rugby, and hockey. The ages affected are usually between 9 and 13 years of age, with girls usually presenting the younger cases. See the left image in Fig. 13 to see why Sever’s can happen in children.
Treating plantar fasciitis
The cause of plantar fasciitis is over-strain on the fibres around the attachment to the heel bone. As made clear here, it occurs most commonly on the inside edge where the fascia’s fibres change their length the most. The origin of the over-strain can arise from many sources, which makes choosing the correct treatment programme more difficult.
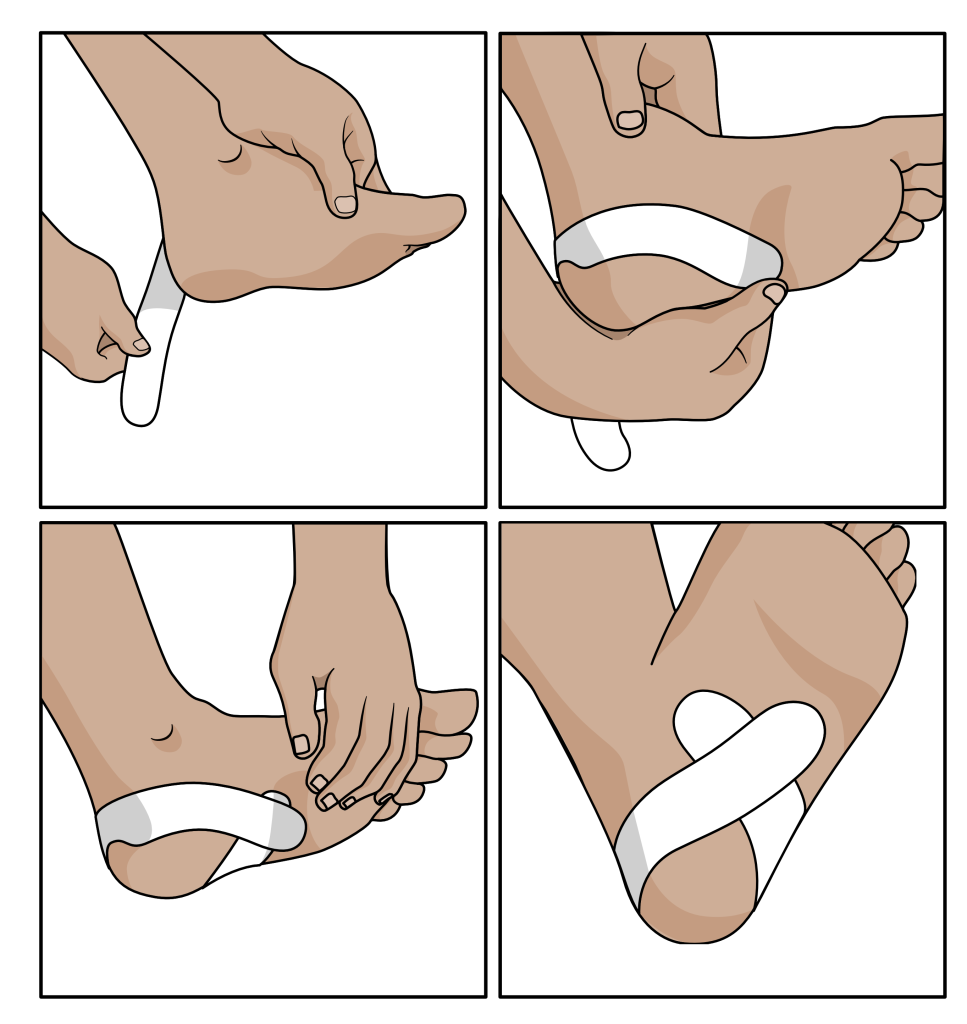
Evidence for the use of foot rehabilitation exercises is high and pain relief can effectively be achieved through strapping around the heel with stretch-resistant tape. See Fig. 18. This may also help to directly reduce stresses on the injured fascia. The application of a cold pack or massaging the area can provide pain relief but does not help healing. The correct shoe choice is also important, and insoles often help reduce pain during and after weight-bearing.
Figure 18. Taping the heel and arch is a tried and tested way to reduce plantar fasciitis pain.
Insoles (foot orthoses/orthotics) have been repeatedly shown to improve symptoms of plantar fasciitis. However, studies have been mixed regarding better results when using custom insole (orthoses) over preformed or customised-performed orthoses. Preformed insoles such as the X-Line PF are much cheaper options than the former bespoke ones. As there is no clear proof that one type is better than the other in managing plantar fasciitis, trying something simple first is probably the best option.
For cases that fail to resolve or only slowly improve with footwear changes, foot exercises, tape, and insoles, shock wave therapy appears to be very beneficial.
Steroid injections can resolve pain in the short term but their long-term success as a single intervention is not proven. Although steroid is a most effective pain killer, their use slows healing and will cause damage and weaken the fibres of the plantar fascia. The more steroid injections, the greater the risk of damage from it.
Key Solutions for plantar fasciitis:
- Strengthen the foot muscles using foot exercises:
- Use stable supportive shoes, even in the house
- Use contoured arch supportive insoles until symptoms have resolved for at least 6 months after
- Use taping to moderate pain in the early stages of treatment
- Consider shockwave therapy if symptoms are not improving after 4 weeks treatment with the correct shoes, insoles, taping, and exercises.
Treatment of early (acute) stages:
Treating plantar fasciitis is far easier if it is caught early because within the first six weeks, a cycle of chronic healing and re-damage has not yet established itself. Therefore, if strains on the plantar fascial attachment can be reduced a little, healing should be able to complete. It’s a case of tipping the balance of stresses towards lower stresses that will promote healing over further damage.
At the first sign of heel pain, try and reduce your weightbearing activities by around 40 % and start to strengthen your foot muscles at least twice a day:
Avoid thin-soled, flat, soft, and flexible shoes. Lace-up comfort styled shoes or boot with a small raise in the heel (rather than completely flat) are by far the best option, which includes trainers that only flex across the toe area.
Supportive boots and trainers offer some of the best footwear options to help with plantar fasciitis.
Consider using a simple ‘arch’ supporting insole, such as the X-Line PF® plantar fasciitis insole healthystep.co.uk/shop/x-line/x-line-pf-insole until the pain completely resolves and for six months after. In the long term, considering using an Arch Angel® insole within footwear you wear when active.
If longer periods of exercise/standing are necessary (for example, at work), strapping the heel will help reduce symptoms and may reduce the amount of strain on the plantar fascia, preventing further damage during these periods. Strapping packs are available but consider the HeelFixKit™ which contains the insoles, tape, and exercise ball required for treating plantar fasciitis.
Treatment of late (chronic) stages:
After 6 weeks of experiencing plantar fascial symptoms, it is highly likely that a chronic cycle of partial healing and re-damaging has become established. It is now essential to reduce strains significantly on the plantar fascia for healing to progress. The heel fix kit™ contains everything you require to start treatment
Reduce weightbearing activity by 50% or more if possible and start foot muscle strengthening exercises 3 to 4 times daily.
Avoid thin-soled, flat, soft flexible shoes. Lace-up comfort styled shoes are by far the best option, which includes trainers that only flex across the toe area (see figure?). Wear these types of shoes in the house as well as outside. Avoid barefoot as much as possible.
Use the X-Line PF® plantar fasciitis insole healthystep.co.uk/shop/x-line/x-line-pf-insole as much as you can. If using the X-line PF® insole does not reduce pain by at least 40% after 4 weeks, a customised preformed insole may work better. For this you’ll need to consult an expert in the treatment of plantar fasciitis.
NOTE: Be cautious if a clinician only offers to scan your foot to provide you with a fully custom insole. There is no convincing evidence that digitally printed insoles provide a superior treatment to any other form of insole, but it will cost far more than most other options. The foot constantly changes shape during gait, with no specific foot position being known to be the ‘best’ shape. Therefore, taking a laser scan of the foot in ‘one’ particular position does not necessarily improve comfort or function during walking or running.
Strapping the heel every other day for 2 weeks usually provides pain relief and should reduce plantar fascial strains. Supplies of heel strapping tape can be order in different quantities as required.
The HeelFixKit™ is an ideal starting pack for plantar fasciitis treatment, with addition tape and insoles available to maintain treatment for longer periods if necessary. It is widely used in the UK within the National Health Service.
If the correct footwear, rehabilitation exercises, insoles, and strapping of the heal are used but fail to improve symptoms by 60% or more over 6 weeks, further treatment should be considered.
Shock wave therapy by a trained clinician is proving to be highly effective, particularly in cases that aren’t settling by simpler techniques. Other options such as steroid injections and surgery should only be considered as last resorts.
- Only consider steroid if other treatments have failed
- Only consider surgery if all other treatments have failed.
The good news is that over a two-year period, 98% of plantar fascial cases will resolve. However, the earlier you can start to protect your plantar fascia, the quicker it will heal and the less pain you will experience.
Sources of Information
The bulk of the information provide here was sourced from the two medical textbooks. The books are extensively referenced from peer-review medical and scientific literature, and are published by Academic Press, an imprint of Elsevier.
Clinical Biomechanics in Human Locomotion: Origins and Principles.
Andrew Horwood, with contributions from Nachiappan Chockalingam
ISBN 978-0-323-85212-8
Clinical Biomechanics in Human Locomotion: Gait and Pathomechanical Principles.
Andrew Horwood, with contributions from Nachiappan Chockalingam
ISBN 978-0-443-15860-5
Both textbooks are available directly from the publisher or through other online and academic book retailers. They are written for a medical audience with some prior anatomical knowledge.